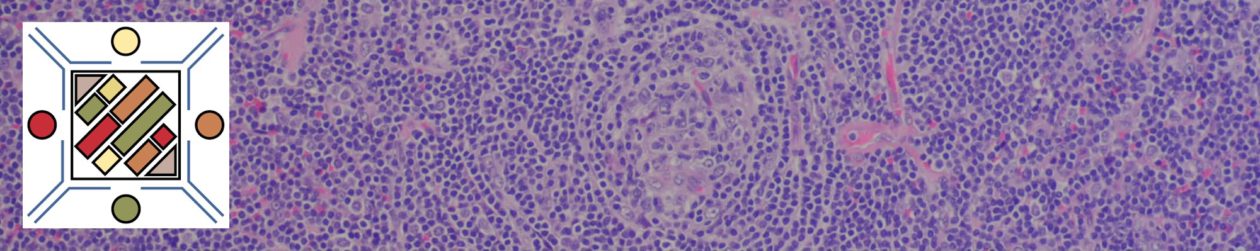
T-Cell/Histiocyte-Rich Large B-Cell Lymphoma (TCHRLBCL) is characterized by spleen and bone marrow involvement. The morphology is of scattered large B-cells with a predominant background composed of T-cell and Histiocytes. The immunophenotype is variable, and an important differential diagnosis is with Hodgkin lymphoma.
Continue reading T-Cell/Histiocyte-Rich Large B-Cell Lymphoma