The most common variant of classical Hodgkin’s lymphoma (65–70% of cases), which is characterized by fibrous collagen bands that divide the lymph node into at least one nodule (fibrosis can range from scant to abundant) and neoplastic Hodgkin cells and Reed-Sternberg (HRS) cells with lacunar morphology (formalin fixation artifact with retraction of the cytoplasm). The lymph node capsule is usually thickened.
Syncytial variant – prominent aggregates of neoplastic Hodgkin cells.
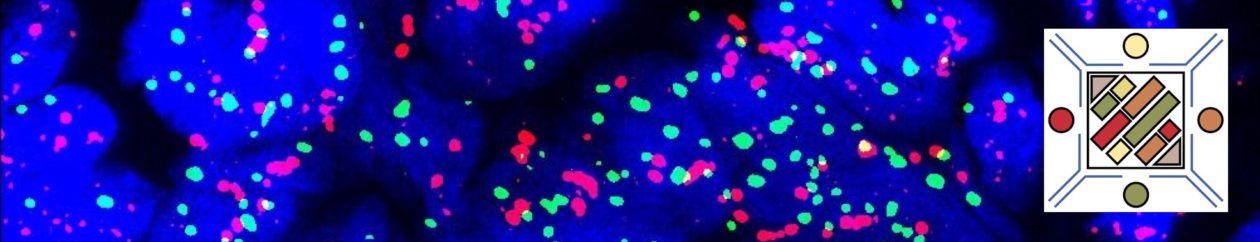
The immunophenotype of nodular sclerosing variant is shared with the other variants of classical Hodgkin lymphoma (PAX-5+, CD15+, CD30+, and CD45-). EBV infection is not common in this subtype (10-40%).
Classical Hodgkin Lymphoma – General Information
Characteristic Immunohistochemical Features
References
Hematopathology. [edited by] Jaffe, ES. 1st. ed. Elsevier, Inc. © 2011.
Robbins and Cotran Pathologic Basis of Disease. V Kumar, et al. 9th Edition. Elsevier Saunders. 2015.
WHO Classification of Tumors of Haematopoietic and Lymphoid Tissues. SH Swerdlow, et al. International Agency for Research on Cancer. Lyon, 2008.