All posts by peferguson
Plasma Cell Neoplasms
2016 WHO Classification
- Monoclonal Gammopathy (MGUS) – IgM
- Monoclonal Gammopathy (MGUS) – Non-IgM
- Plasma Cell Myeloma
- Plasma Cell Myeloma – Variants
- Smoldering Plasma Cell Myeloma (Asymptomatic)
- Non-Secretory Myeloma
- Plasma Cell Leukemia
- Plasmacytoma
- Solitary Plasmacytoma of Bone
- Extraosseous Plasmacytoma
- Monoclonal Immunoglobulin Deposition Disease
Large B-Cell Lymphomas
- Diffuse Large B-Cell Lymphoma (DLBCL), NOS
- Germinal Center B-Cell Type
- Activated B-Cell Type
- Large B-Cell Lymphoma with IRF4 Rearrangement
- T-Cell/Histiocyte-Rich Large B-Cell Lymphoma
- Primary DLBCL of the CNS
- Primary Cutaneous DLBCL, Leg Type
- EBV+ DLBCL, NOS
- DLBCL Associated with Chronic Inflammation
- Primary Mediastinal (Thymic) Large B-Cell Lymphoma
- Intravascular Large B-Cell Lymphoma
- ALK+ Large B-Cell Lymphoma
- Plasmablastic Lymphoma
- HHV-8+ DLBCL, NOS
- Primary Effusion Lymphoma
WHO 2008/2016 Criteria for Mixed-Phenotype Blasts
Myeloid
- MPO expression (flow cytometry, immunohistochemistry, or enzyme cytochemistry) – WHO does not define thresholds for positiivity, which can result in variability between laboratories
- Flow cytometry: >10% (some propose 13%) expression compared to isotype control (preferred methodology)
- Enzyme cytochemsitry: >3% staining of blasts
- IHC: No well-defined cutoff (not commonly done – MPO IHC is available)
Continue reading WHO 2008/2016 Criteria for Mixed-Phenotype Blasts
EGFR Mutations
EGFR mutations are one of the most common mutations in lung adenocarcinomas, which have an approximate 70% response rate to targeted therapy with tyrosine kinase inhibitors (TKI). Continue reading EGFR Mutations
EGIL Algorithm for Biphenotypic Blasts
|
Points
|
B
|
T
|
Myeloid
|
|
2
|
cyCD79a
|
CD3 (cy or sm)
|
MPO
|
|
|
cyCD22
|
TCR-αβ
|
|
|
|
cyIgM
|
TCR-γδ
|
|
|
1
|
CD19
|
CD2
|
CD117
|
|
|
CD20
|
CD5
|
CD13
|
|
|
CD10
|
CD8
|
CD33
|
|
|
|
CD10
|
CDw65
|
|
0.5
|
TdT
|
TdT
|
CD14
|
|
|
CD24
|
CD7
|
CD15
|
|
|
|
CD1a
|
CD64
|
Biphenotypic leukemia is defined as a score >2 in 2 lineage columns.
WHO 2008/2016 Criteria for Mixed-Phenotype Blasts
Mixed Phenotypic Acute Leukemias (MPAL)
References
Bene MC, Castoldi G, Knapp W, et al. Proposals for the immunological classification of acute leukemias: European Group for the Immunological Characterization of Leukemias (EGIL). Leukemia. 1995;9(10):1783–1786
MPAL
- BIPHENOTYPIC – single population of blasts that express key markers of different lineages (e.g. T-ALL, B-ALL, and/or AML).
- BILINEAL – two cell populations each diagnostic of separate acute leukemia lineages (combined populations ≥20% blasts to met threshold for acute leukemia).
Special Subtypes of Breast Carcinoma
-
Lobular Carcinoma
-
Medullary Carcinoma
- Pattern characteristic of BRCA1 associated carcinomas
- 13% are medullary type
- 60% have subset of medullary features
- Well-circumscribed mass
- Solid sheets of pleomorphic large cells containing prominent nucleoli In >75% of the mass
- Frequent mitosis
- Prominent lymphoplasmacytic inflammatory infiltrate surrounding and infiltrating the tumor
- Pushing/non-infiltrating border
- DCIS is minimal or absent
- WHO recommends classifying tumor as “carcinomas with medullary features”
- Pattern characteristic of BRCA1 associated carcinomas
-
Micropapillary Carcinoma
-
Mucinous (colloid) carcinoma
-
Tubular Carcinoma
-
Papillary Carcinoma
-
Secretory Carcinoma
-
Inflammatory Carcinoma
- Clinically present with breast erythema and thickening (peau d’orange)
- Dermal lymphatics filled with tumor
- 3-year survival rate 3-10%
-
Neuroendocrine Tumors
- Well-differentiated Neuroendocrine Tumor
- Small Cell Carcinoma
References
Kumar, Vinay, Abul K. Abbas, and Jon C. Aster. Robbins and Cotran Pathologic Basis of Disease. Ninth edition. Philadelphia, PA: Elsevier/Saunders, 2015.
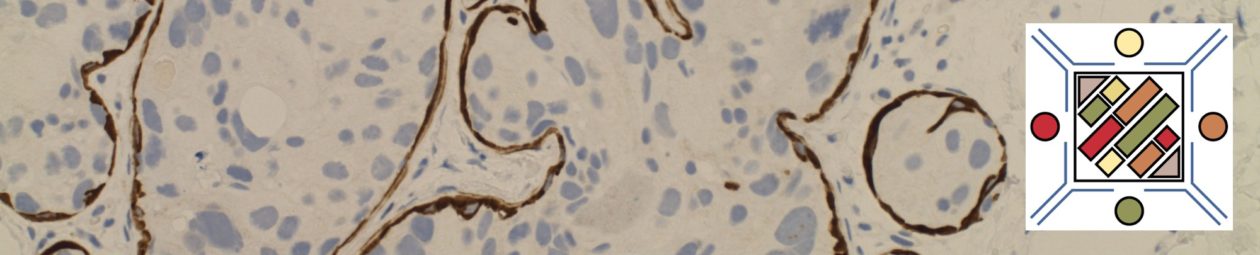
Lung IHC
Many different markers can be used in neoplastic lung, but the most common involve differentiation between squamous and adenocarcinoma and identifying evidence of neuroendocrine differentiation. Continue reading Lung IHC