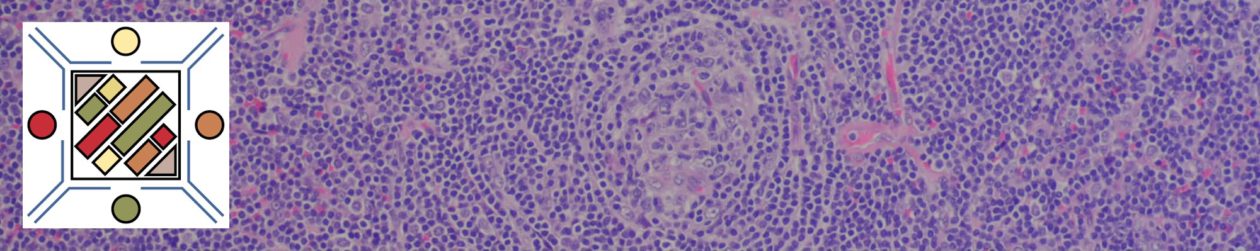
Not infrequently in breast pathology, the differential diagnosis of micro-invasion vs. DCIS or a scerlosing lesion +/- tubular carcinoma will occur. These type of cases can be very challenging based just on H&E morphology. Fortunately, there are multiple IHC markers, which can be helpful in identifying the myoepithelial layer. The main pitfall in interpretation of most of these markers, is that they will also mark myofibroblasts (on occasion) in the intervening stroma. When this occurs, and myofibrilblasts abut the glands, the staining pattern can be misinterpreted as an intact myoepithelial layer.
|
Antibody
|
MEC
|
Myofibroblasts
|
|
++++
|
++
|
|
|
++++
|
++
|
|
|
SMA
|
++++
|
+++
|
|
p63 (nuclear)
|
++++
|
–
|
|
++++
|
–
|
|
|
+++
|
+
|
|
|
++
|
–
|
SMA = Smooth Muscle Action, SMM-HC = Smooth Muscle Myosin Heavy Chain.
The most commonly used stains include SMM-HC, calponin, CK5, and p63. p63 can be combined with any of the other cytoplasmic stains as part of a double stain protocol. SMA is the most proned of the stains to also mark fibroblasts. S-100 is NOT recommended as a myoepithelial marker. p63 has the least association with myofibroblast staining, but expression may be discontinuous in the myoepithelial cells layer, which can lower sensitivity when used alone. In the opinion of many breast pathologists, SMM-HC as a single stain probably has the best combined sensitivity for the myoepithelial cells with minimal myofibroblastic staining, but many will use multiple markers in difficult cases.
Myofibroblast Staining
Actin > Calponin > SMM-HC
References
Hicks DG. Immunohistochemistry in the diagnostic evaluation of breast lesions. Appl Immunohistochem Mol Morphol. 2011;19(6):501–505. doi:10.1097/PAI.0b013e31822c8a48.
Liu H. Application of immunohistochemistry in breast pathology: a review and update. Arch Pathol Lab Med. 2014;138(12):1629–1642. doi:10.5858/arpa.2014-0094-RA.