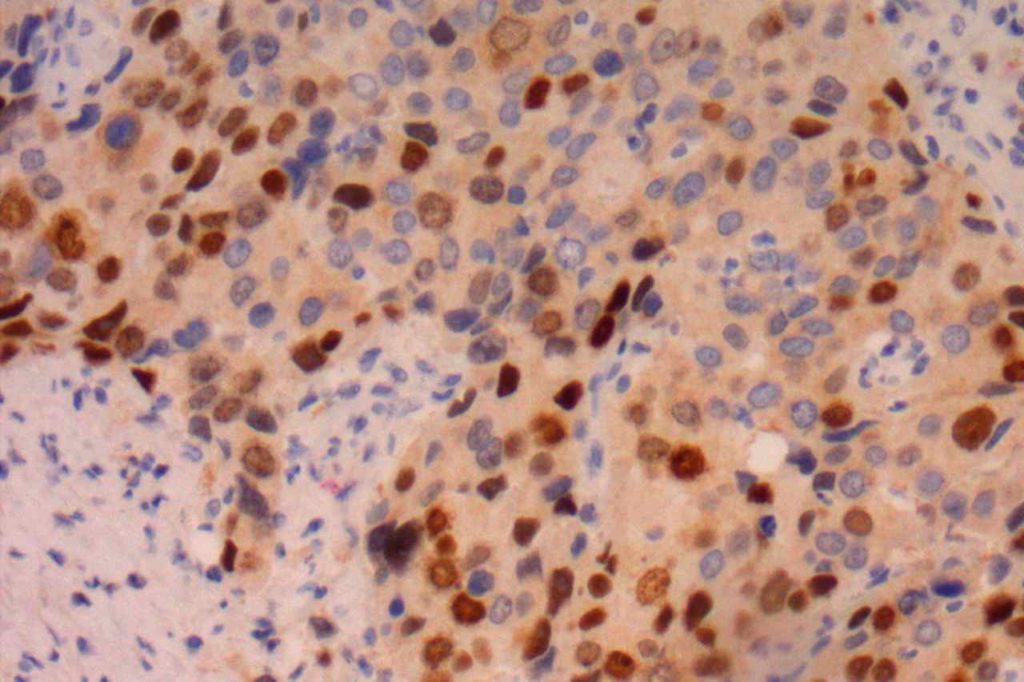
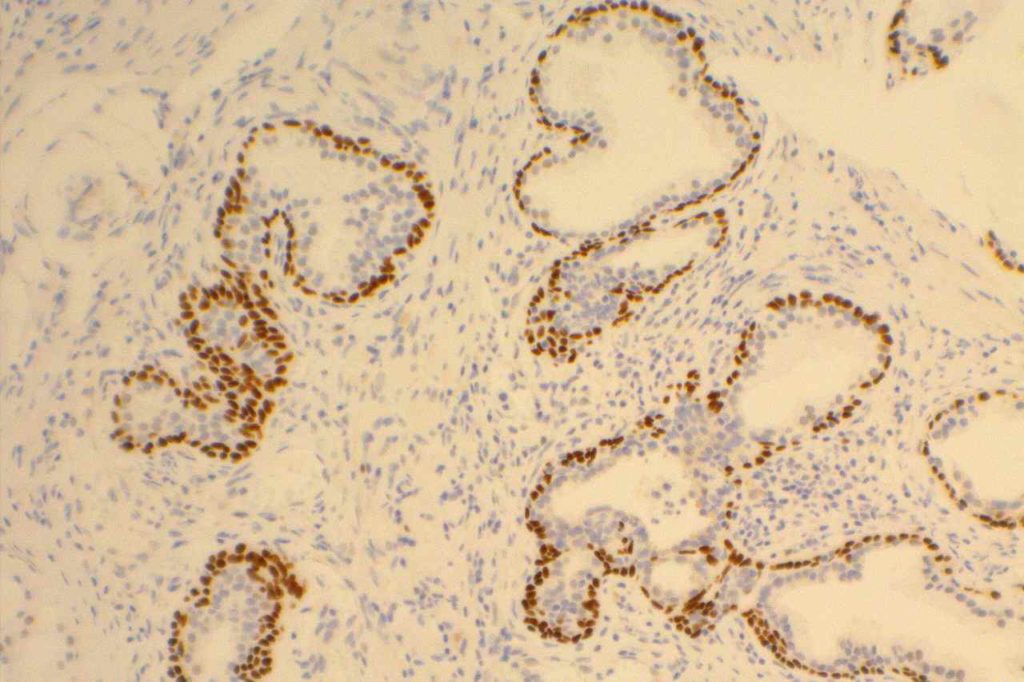
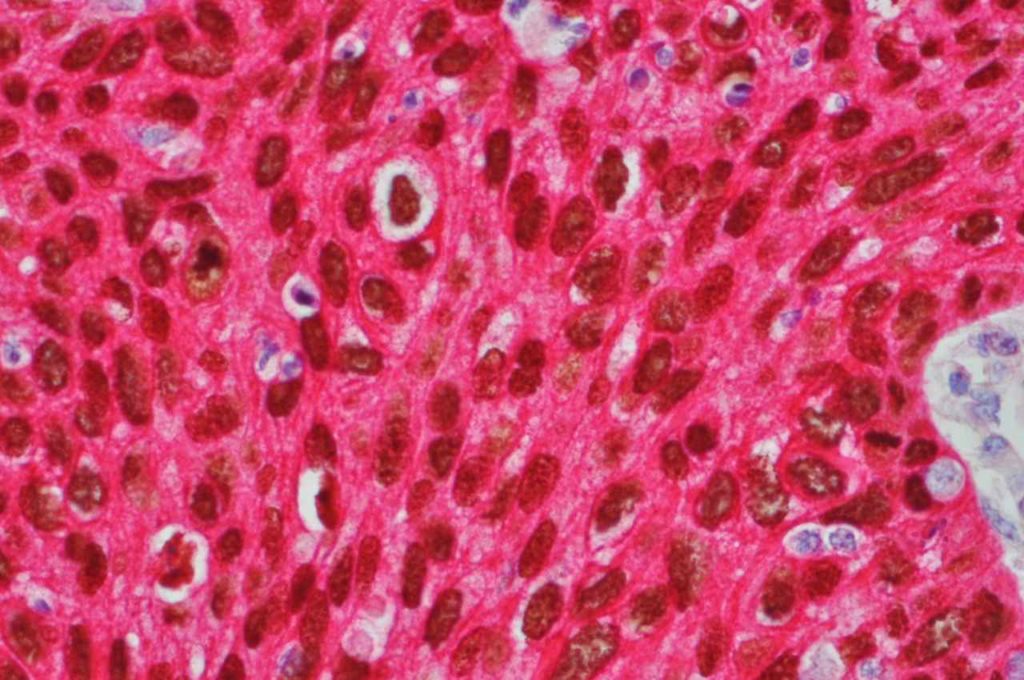
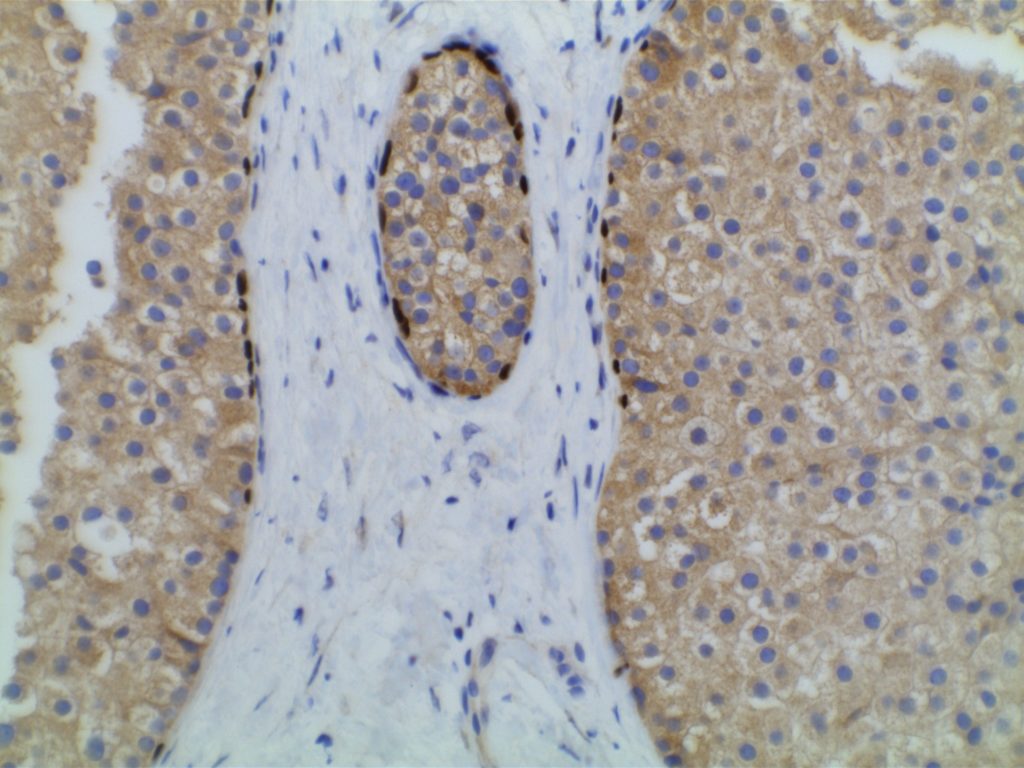
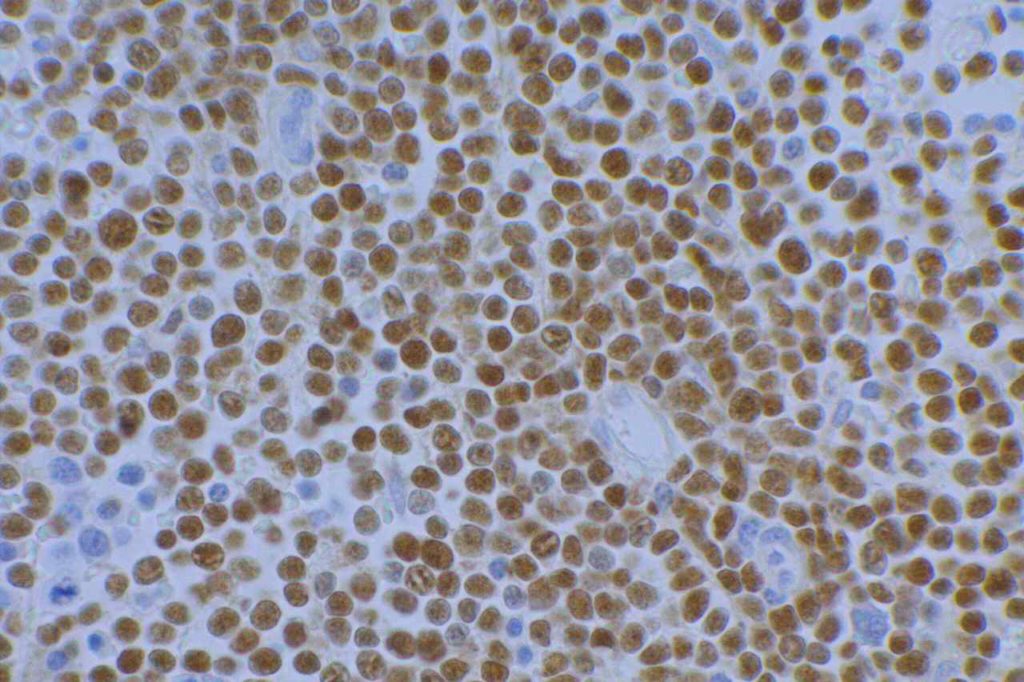
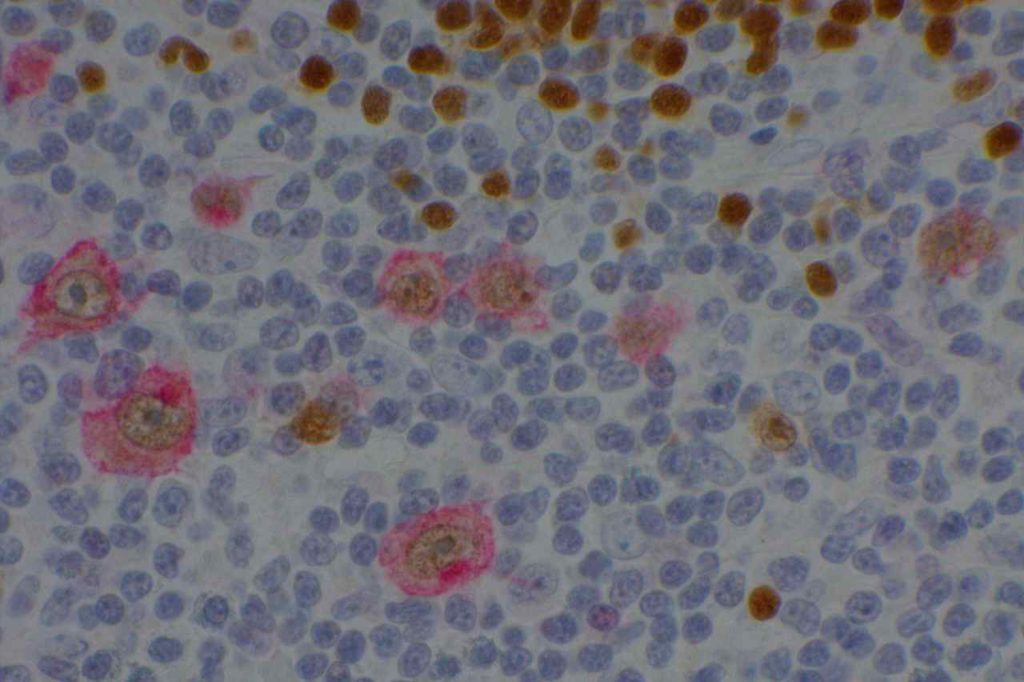
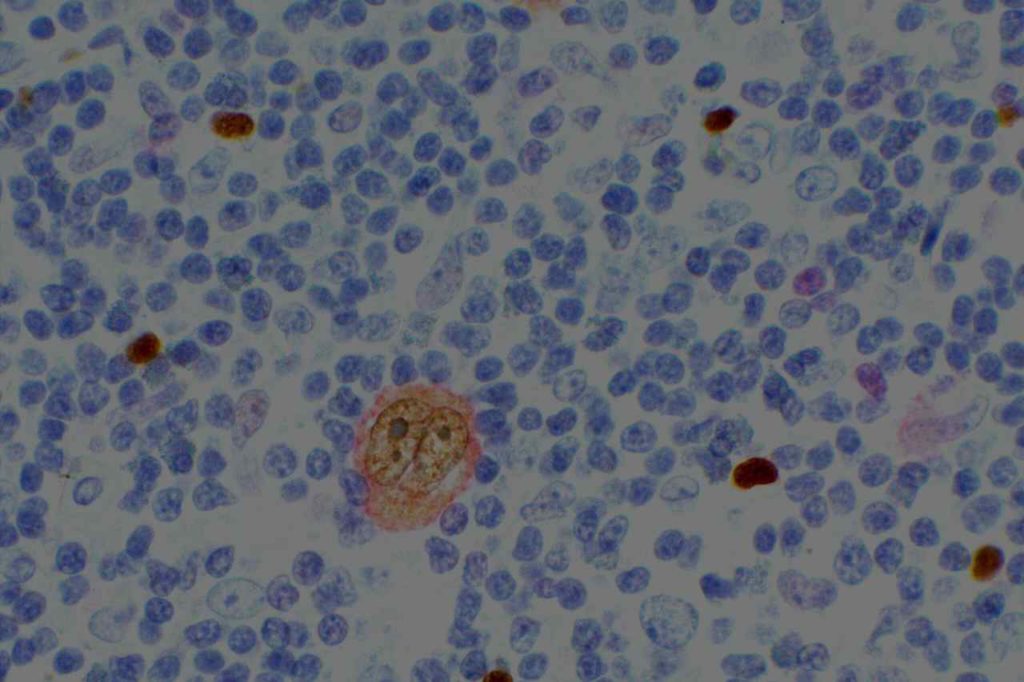
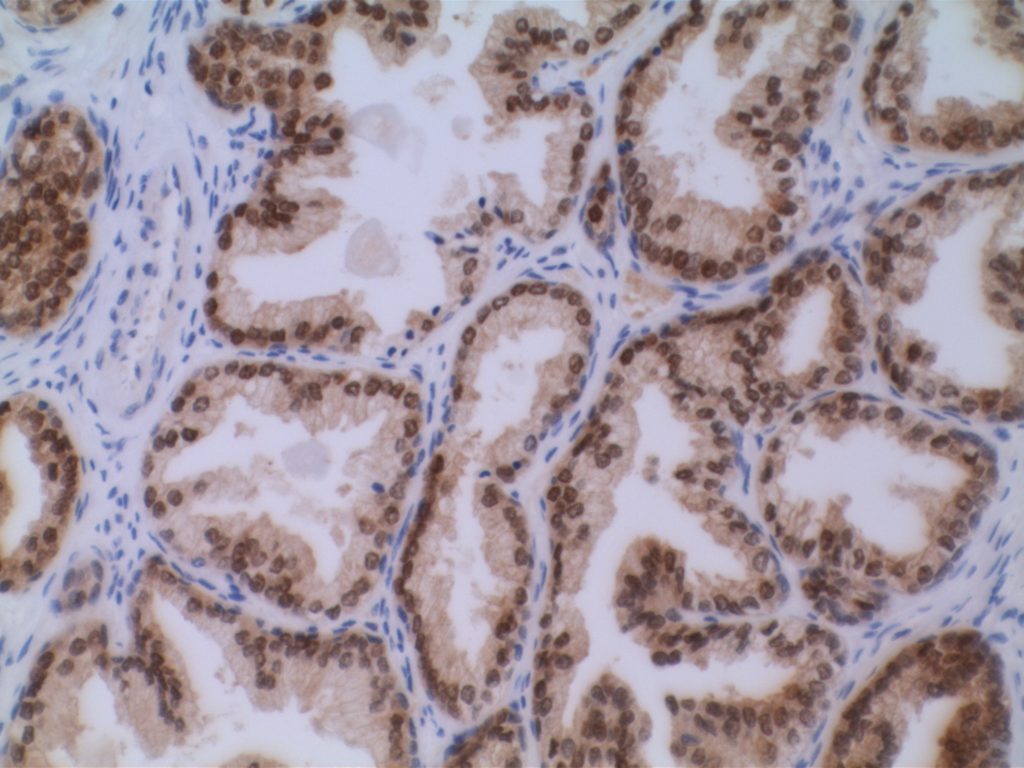
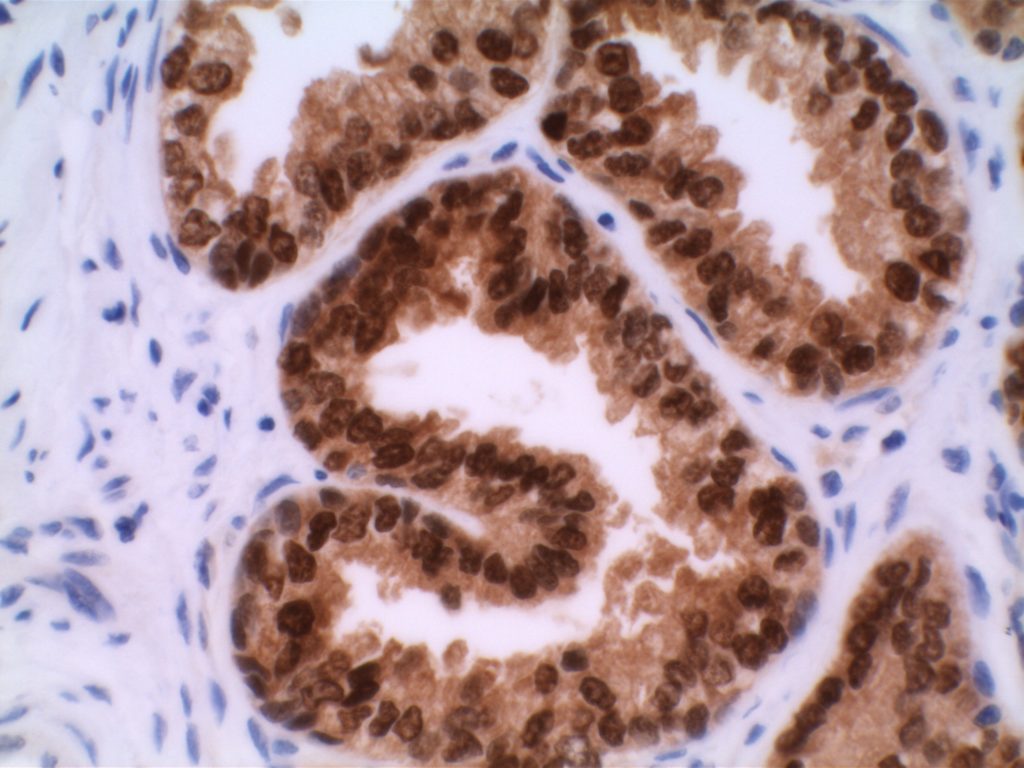
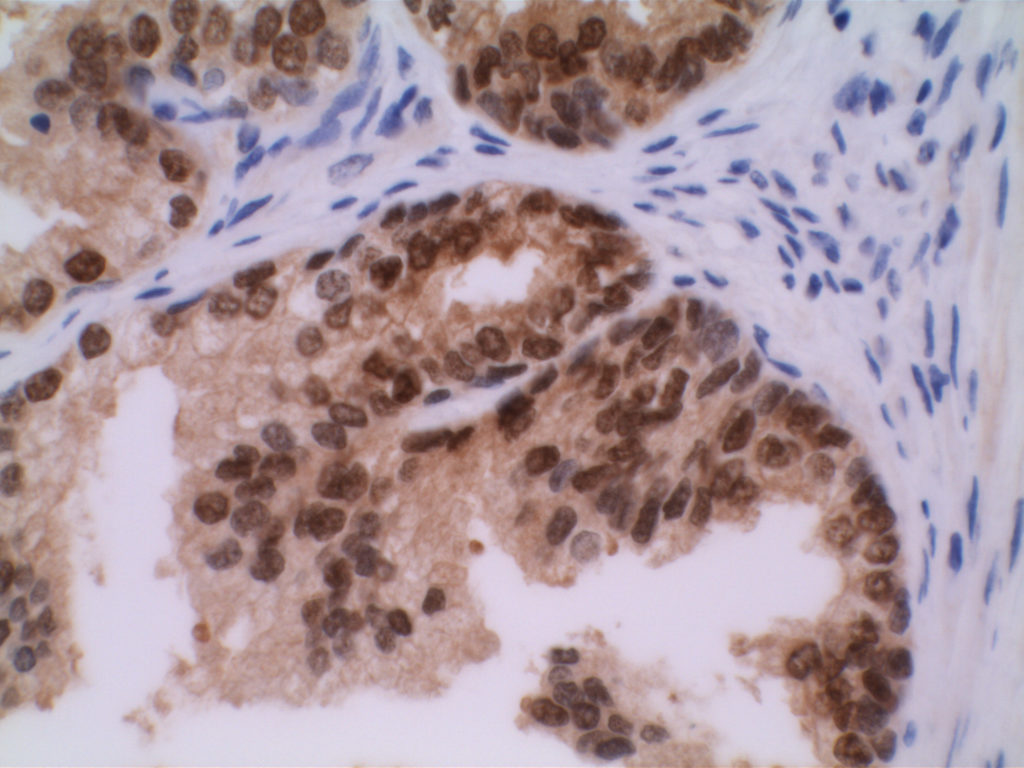
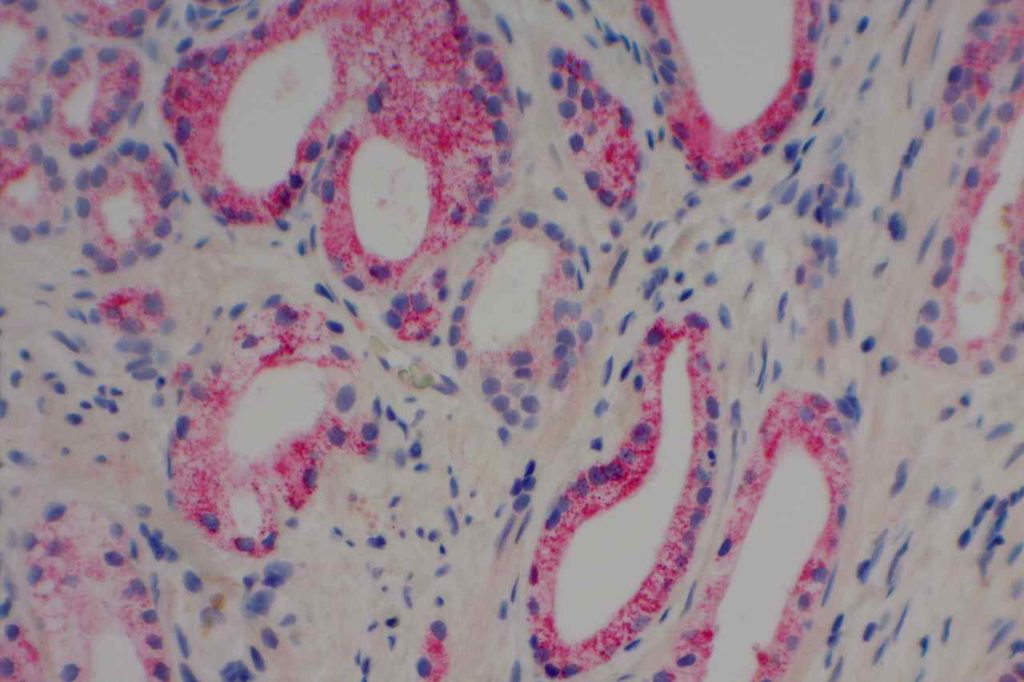
PIN-4 is a cocktail stain used in evaluation of prostate specimens, and contains antibodies CK5, CK14, p63, andP504S. CK5 and CK14 are high molecular weight keratins, which are expressed in the basal layer of normal prostate glands. p63 is also expressed in the nuclei of prostate basal epithelial cells. Therefore, combining p63, CK5 and CK14 allows to increase the sensitivity in identifying a basal epithelial layer in prostate glands. The absence of a basal epithelial layer around prostate epithelium is characteristic of an invasive prostate adenocarcinoma.
P504S is a racemase (AMACR), which is over-expressed in a significant percentage of prostate adenocarcinomas and high-grade-PIN. Benign glands do not typically express P504S with rare exceptions. It is also important to understand that P504S, while demonstrating good specificity for benign versus neoplastic prostate gland epithelium, is NOT specific to only neoplastic prostate epithelium. Other (non-prostate) benign and neoplastic processes may express P504S (e.g. nephrogenic adenoma).
Microscopic Images


References
Yang, X. J., Wu, C.-L., Woda, B. A., Dresser, K., Tretiakova, M., Fanger, G. R., & Jiang, Z. (2002). Expression of alpha-Methylacyl-CoA racemase (P504S) in atypical adenomatous hyperplasia of the prostate. The American Journal of Surgical Pathology, 26(7), 921–925. doi:10.1097/01.PAS.0000017328.13364.17
Luo, J., Zha, S., Gage, W. R., Dunn, T. A., Hicks, J. L., Bennett, C. J., et al. (2002). Alpha-methylacyl-CoA racemase: a new molecular marker for prostate cancer. Cancer Research, 62(8), 2220–2226.
Zhou, M., Chinnaiyan, A. M., Kleer, C. G., Lucas, P. C., & Rubin, M. A. (2002). Alpha-Methylacyl-CoA racemase: a novel tumor marker over-expressed in several human cancers and their precursor lesions. The American Journal of Surgical Pathology, 26(7), 926–931. doi:10.1097/01.PAS.0000018309.60184.52
Tacha, D. E., & Miller, R. T. (2004). Use of p63/P504S monoclonal antibody cocktail in immunohistochemical staining of prostate tissue. Applied Immunohistochemistry & Molecular Morphology : AIMM / Official Publication of the Society for Applied Immunohistochemistry, 12(1), 75–78.
Jiang, Z., Li, C., Fischer, A., Dresser, K., & Woda, B. A. (2005). Using an AMACR (P504S)/34bE12/p63 Cocktail for the Detection of Small Focal Prostate Carcinoma in Needle Biopsy Specimens. American Journal of Clinical Pathology, 123(2), 231–236. doi:10.1309/1G1NK9DBGFNB792L