CK5 is a high molecular weight cytokeratin that stains stratified squamous epithelium (e.g. skin, tongue mucosa, etc.), basal cells of the prostate gland, myoepithelial cells in breast tissue, and mesothelial cells/mesothelioma. Therefore CK5 is an excellent marker, which can be used in a variety of diagnostic applications.
CK5 is useful in the diagnosis of squamous cell carcinoma, urothelial carcinoma, mesothelioma, thymic tumors, and skin appendage tumors. It is also helpful in identifying the myoepithelial layer in breast tissue, and the basal layer in prostate tissue.
The combined expression of p63 and CK5 in poorly differentiated tumors is highly suggestive of squamous origin (Kaufmann, O., et al)
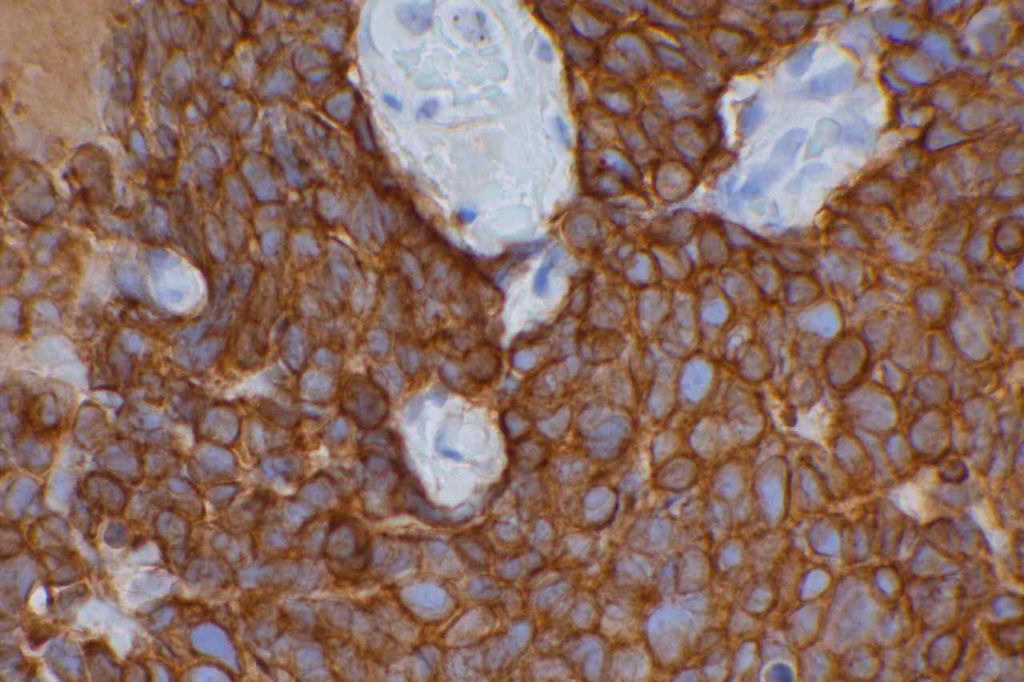
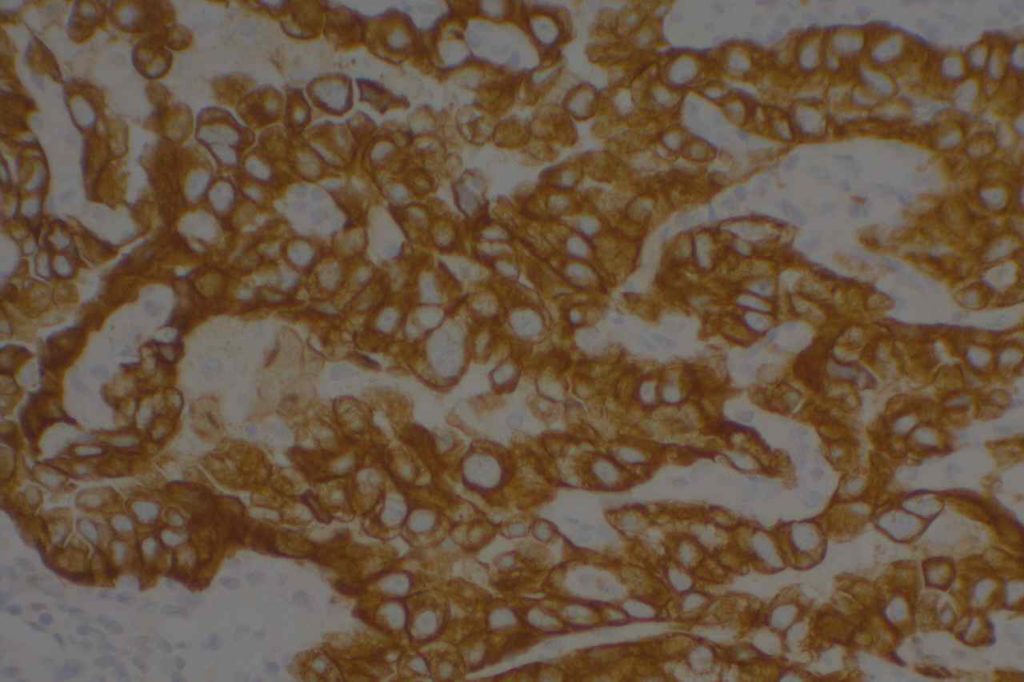
Lung
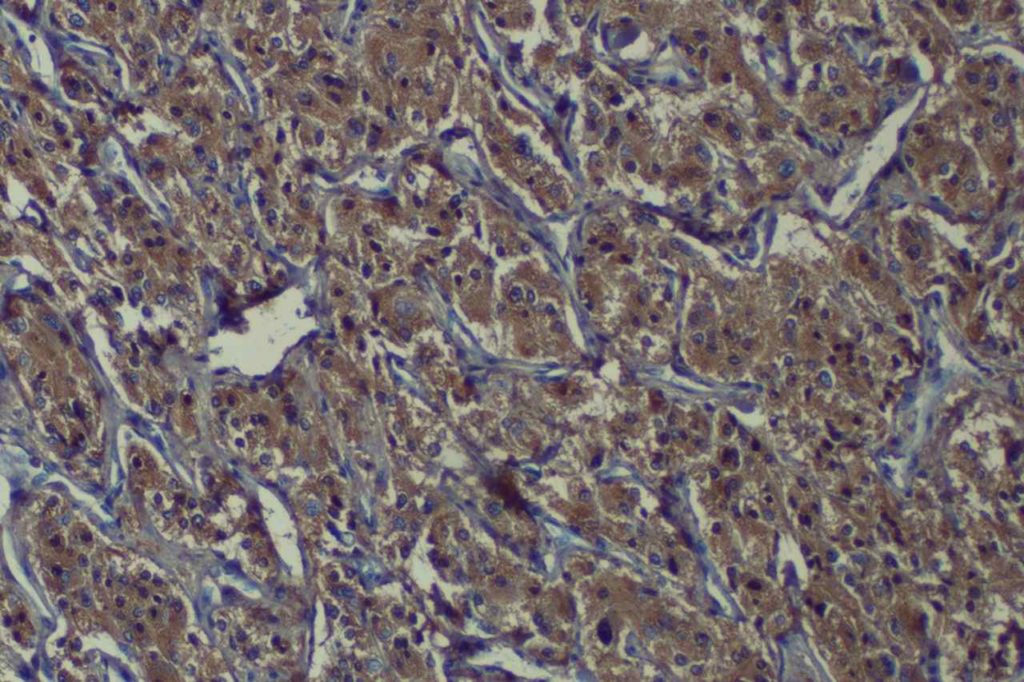
CK5 will stain approximately 70-80% of squamous cell carcinomas with a cytoplasmic staining pattern. p63 is considered slightly more sensitive, but may give varying positivity in cases of lung adenocarcinoma that can be confusing. Therefore, CK5 and p63 are often used as part of a panel to diagnose squamous cell carcinoma. Since p63 is a nuclear marker, these two stains can be performed as a double stain on a single slide with one or two different chromogens.
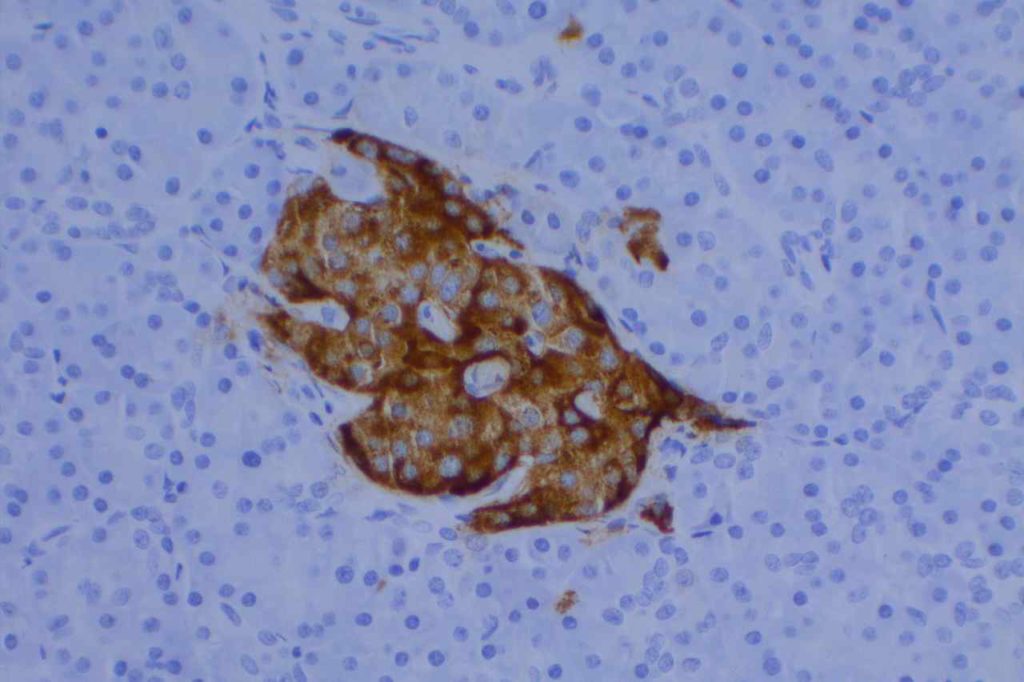
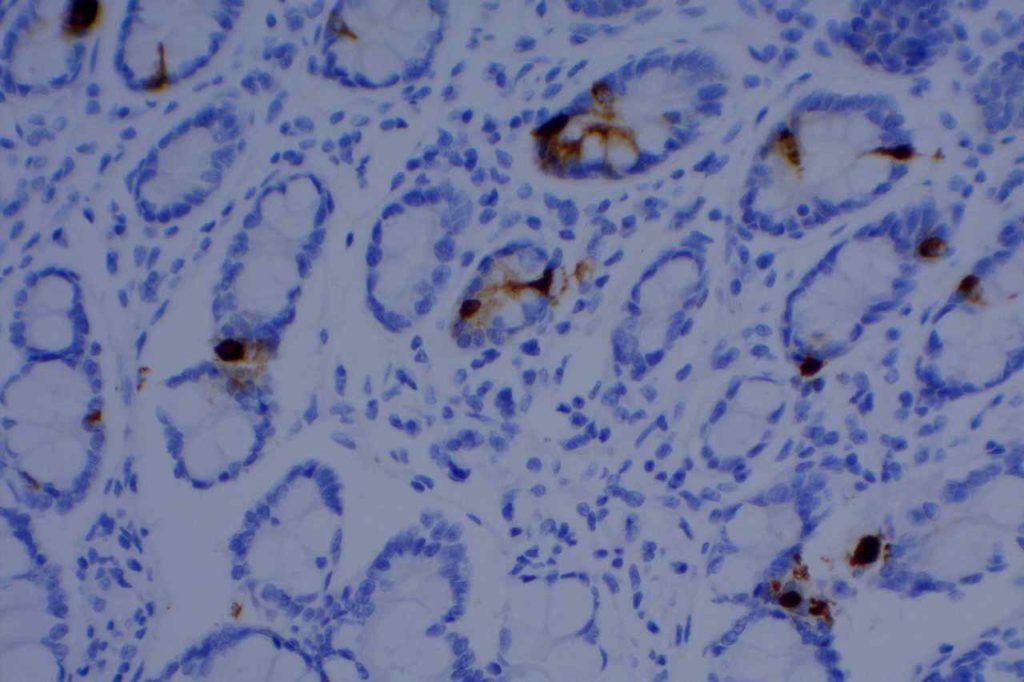
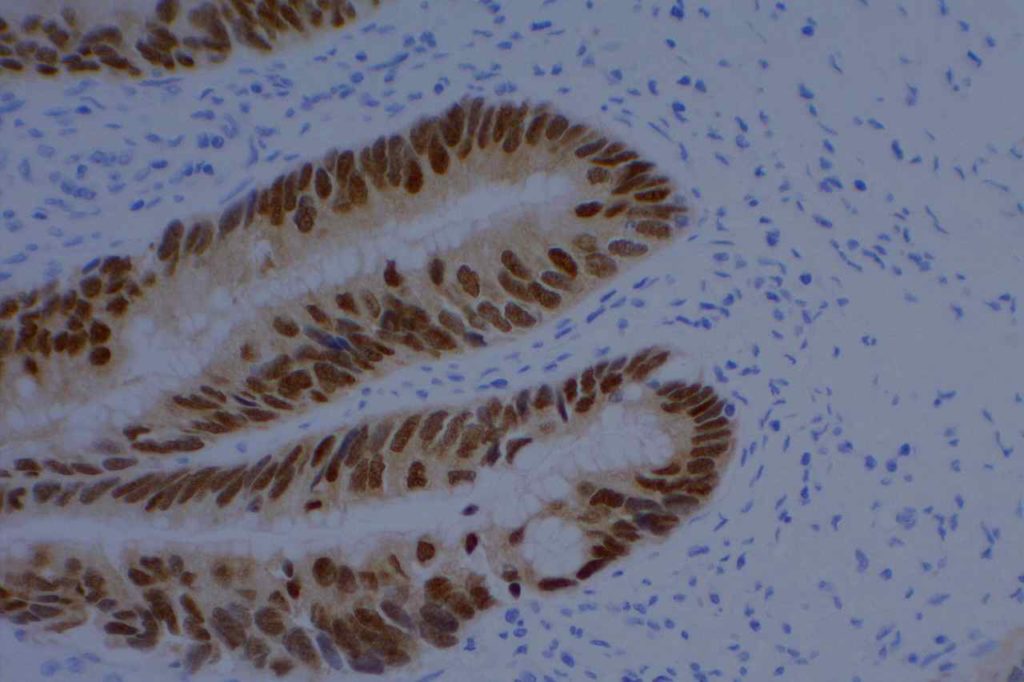
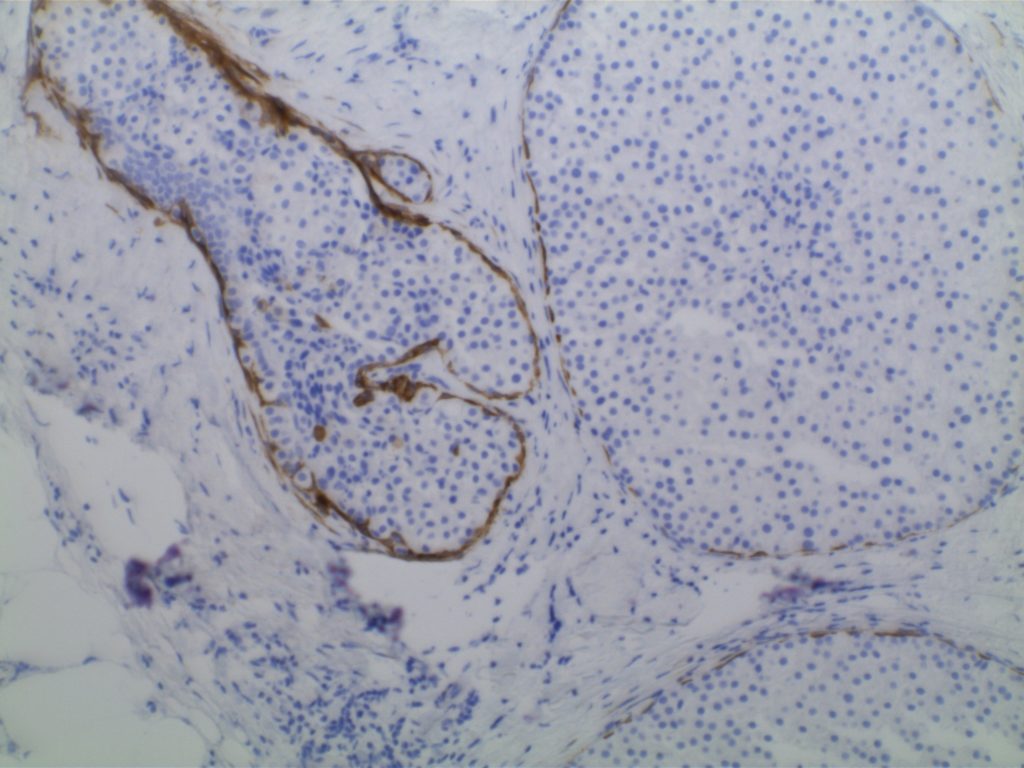
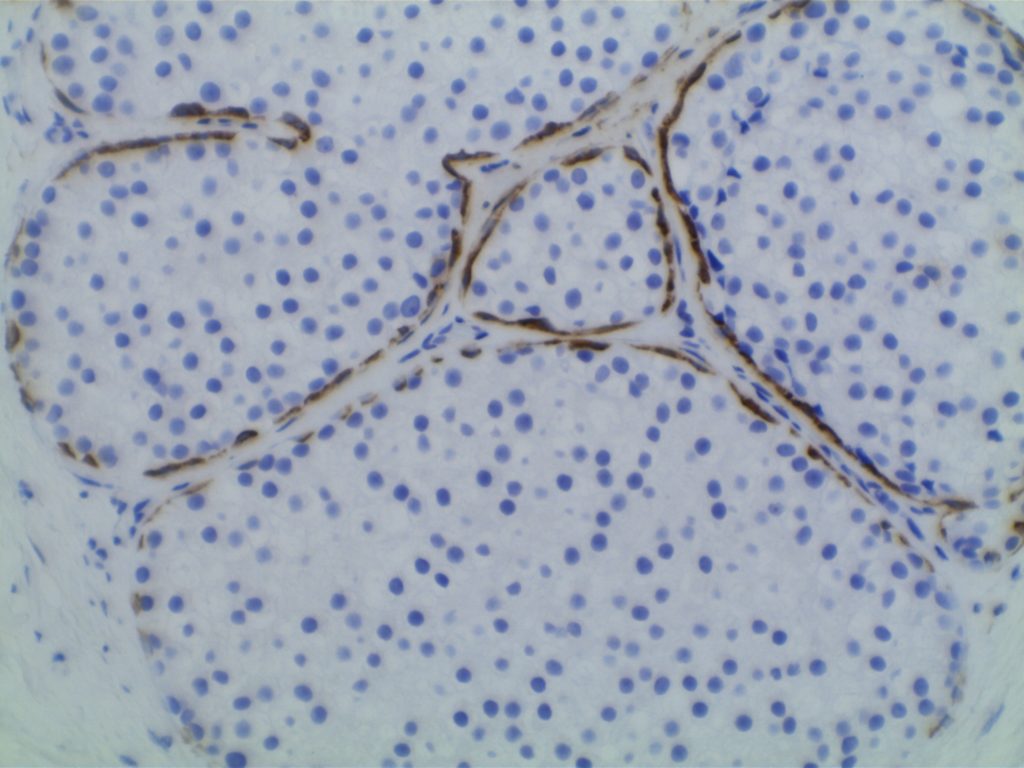
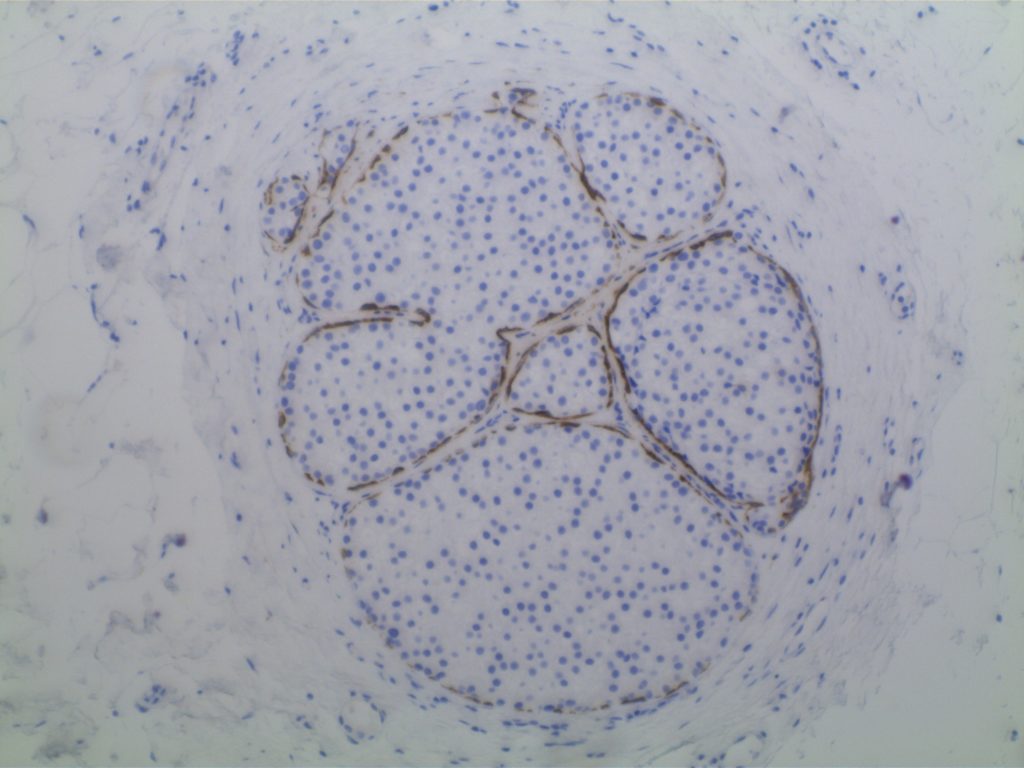
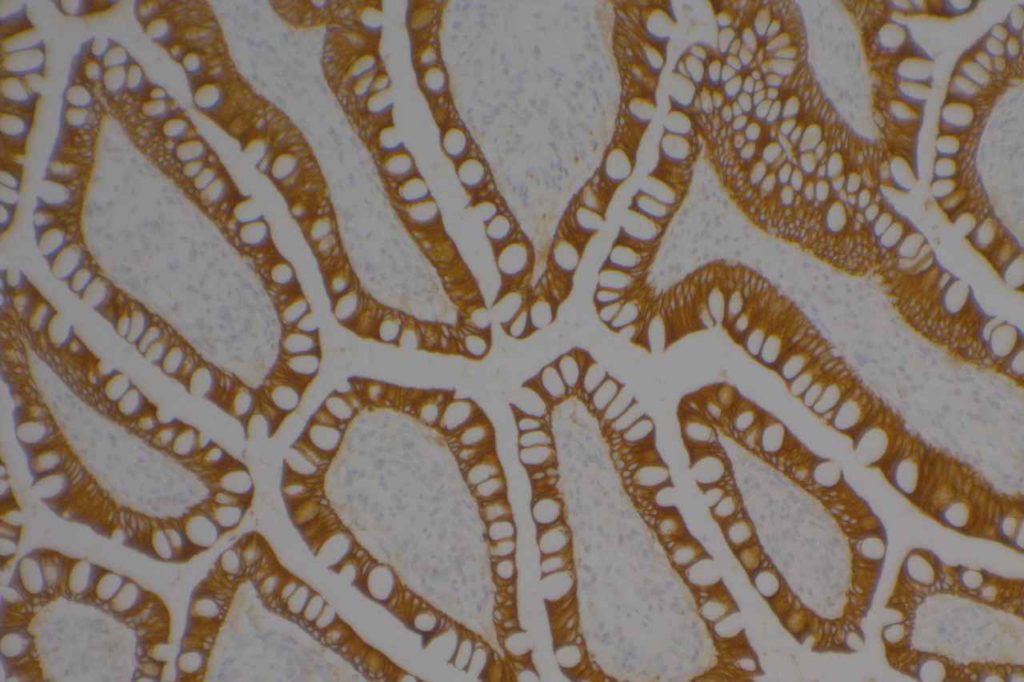
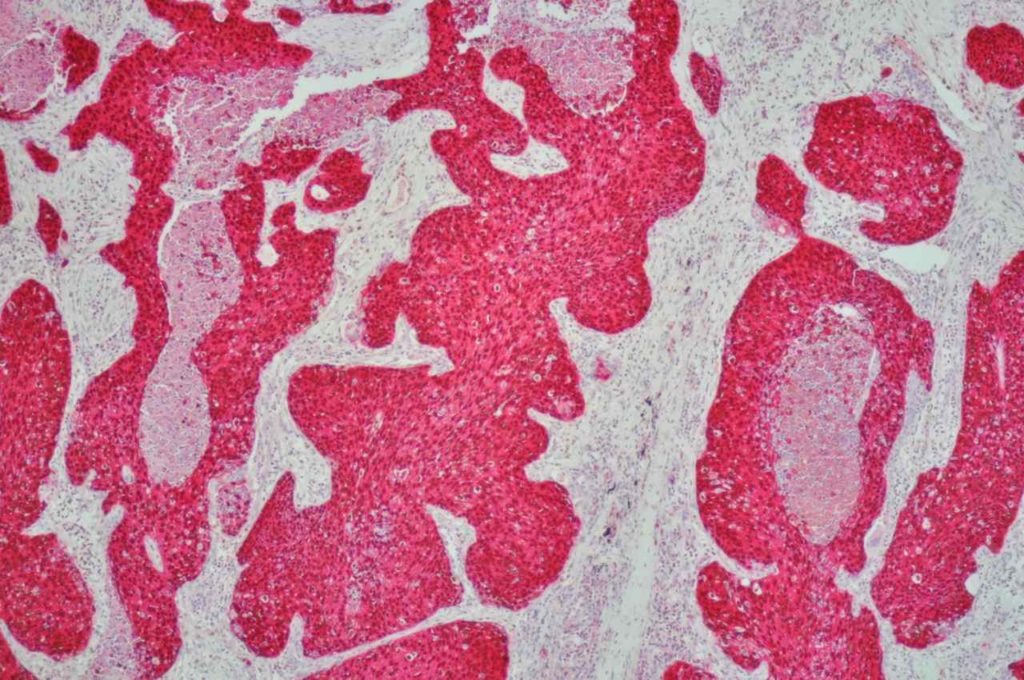
Prostate
CK5 is an excellent marker for the basal layer, and stains in a similar pattern to 34βE12. Again, CK5 can be combined with p63, which also stains the basal layer of prostate glands.
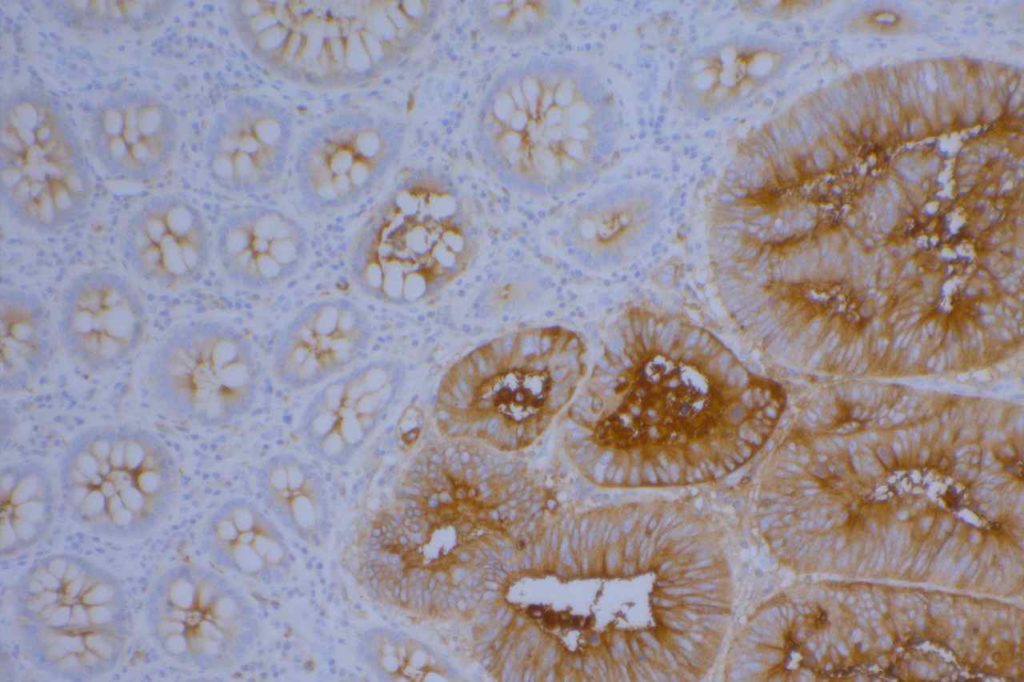
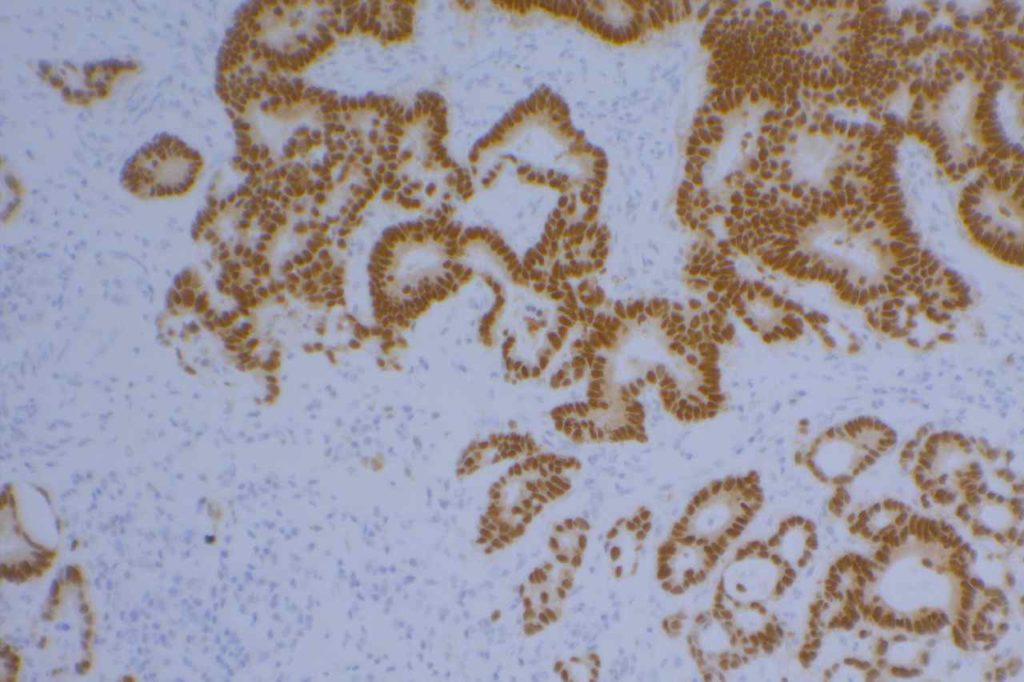
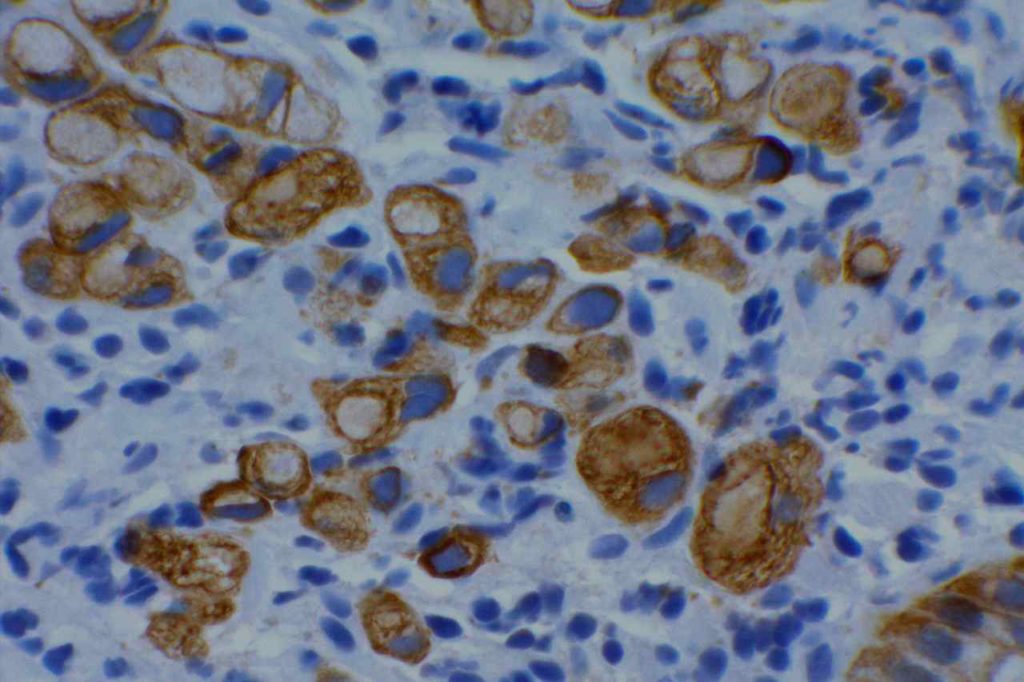
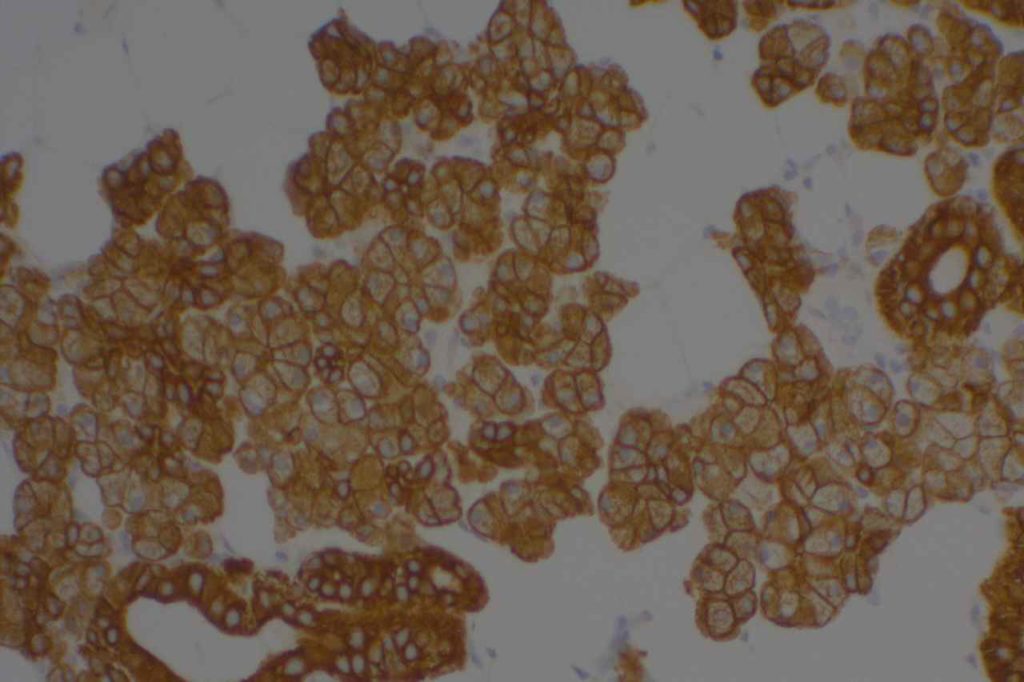
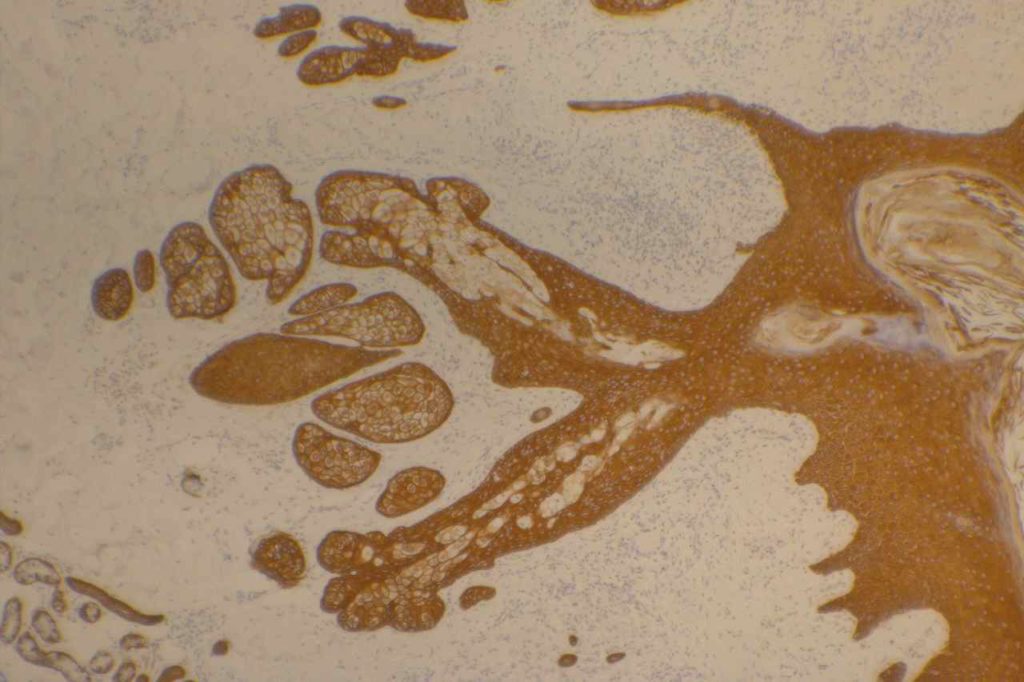
Bladder
Urothelial carcinoma will typically express p63 diffusely with variable reports of CK5 or CK5/6 expression in urothelial carcinoma.
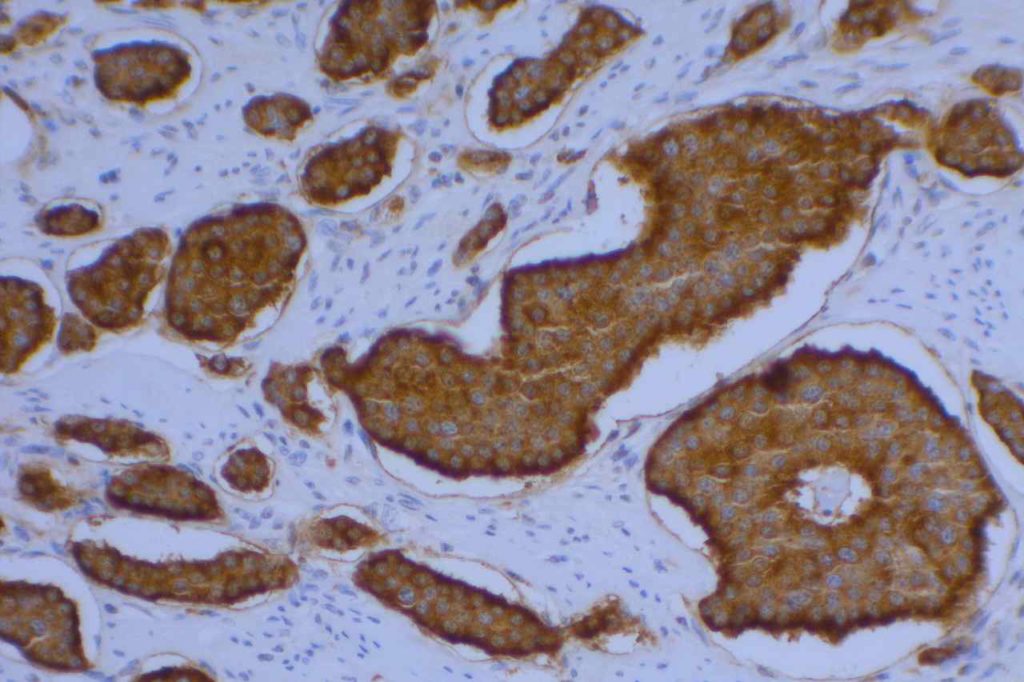
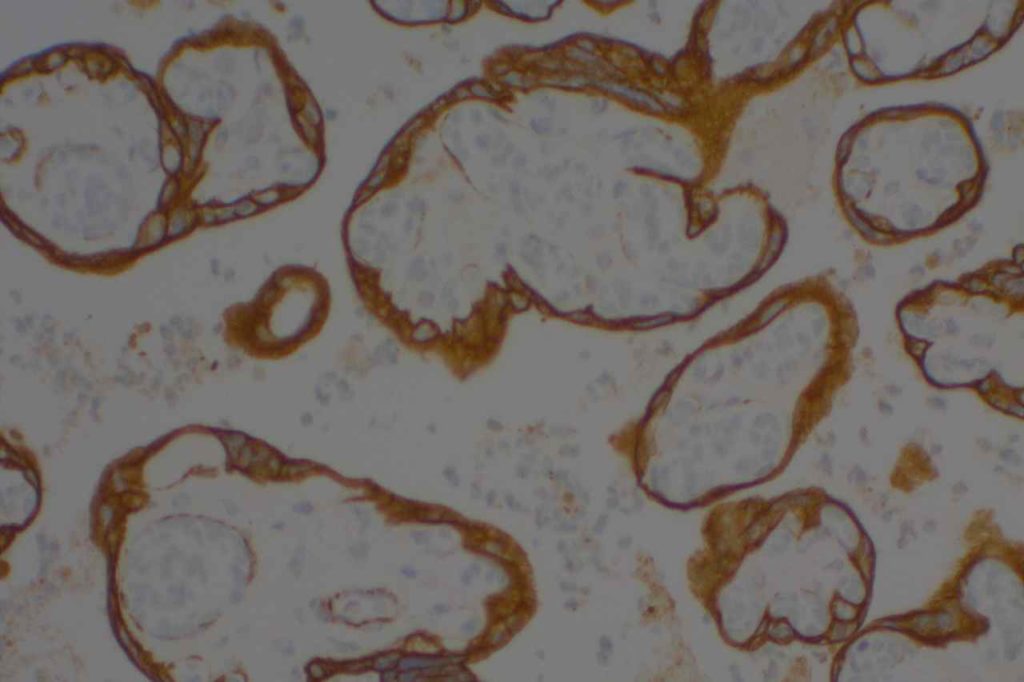
Breast
CK5 will stain the myoepithelial layer of breast tissue, but other markers such as smooth muscle myosin and calponin are typically used more commonly. Basal-like breast carcinomas usually express CK5, especially with the monoclonal CK5 antibody compared to CK5/6 (Bhargava, R, et al). Metaplastic/sarcomatoid breast carcinomas have also been reported to express CK5.
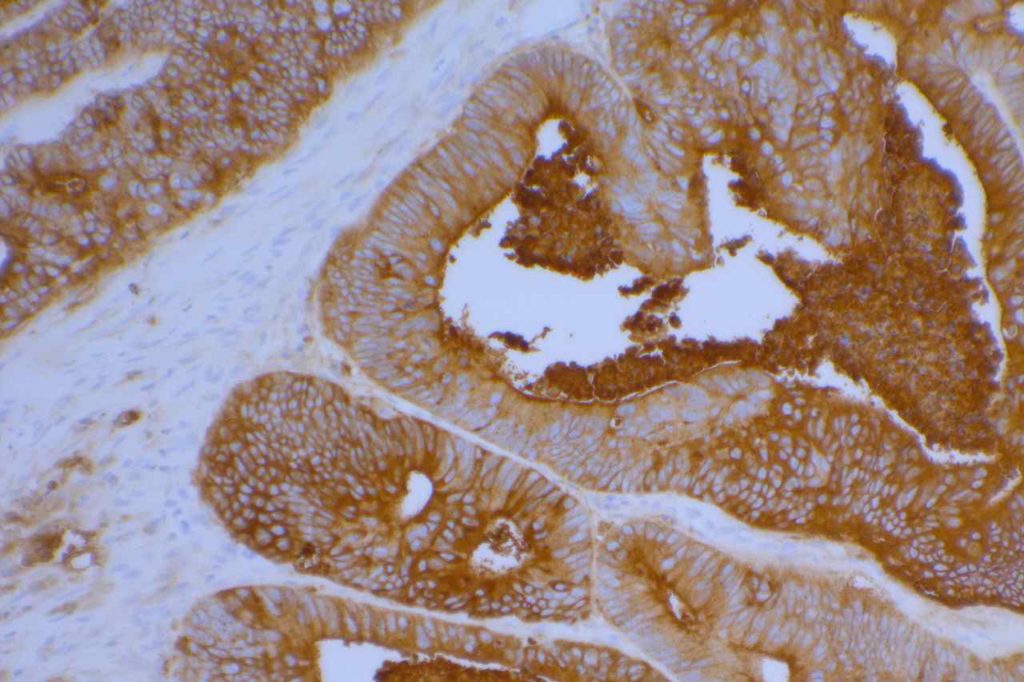
Skin
CK5 will stain the stratified squamous epithelium. If there are cells in the squamous epithelium, which may be Paget cells or melanocytes, CK5 can be used along with CK7 or Melan A/HMB-45 to differentiate between odd appearing keratinocytes, Paget’s disease, or melanocytes.
CK5 vs. CK5/6
There is occasionally discussion as to which is a better marker. Some feel CK5/6 is a better marker since it has more than one cytokeratin in it’s cocktail. However, there is a very strong consensus among pathologists who have used both that CK5 performs significantly better than CK5/6, and is therefore, the preferred antibody.
Common expression patterns in carcinoma (Chu, PG, et al).
|
Tumor
|
Expression %
|
Differentiation
|
|
Skin: BCC & SCC
|
100%
|
Squamous
|
|
Squamous Salivary Gland Tumors
|
100%
|
Myoepithelial
|
|
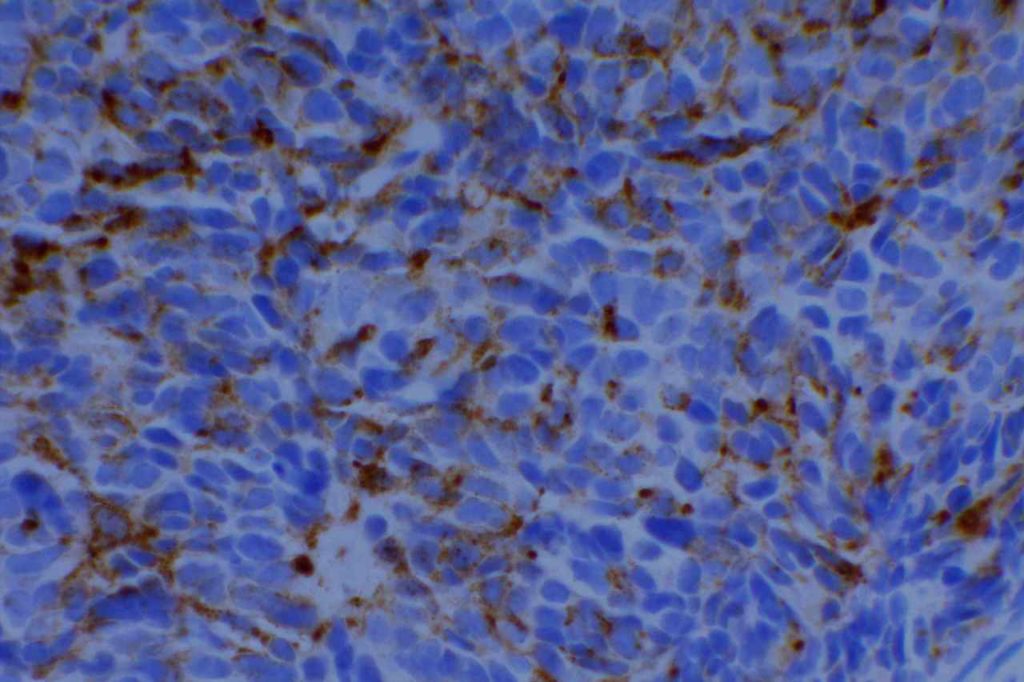
Mesothelioma
|
76%
|
Mesothelial
|
|
Urothelial Ca.
|
62%
|
Transitional
|
|
Endometrial Ca.
|
50%
|
Squamous
|
|
Ovarian Ca. (Serous)
|
75%
|
Serous Epithelium
|
Note: other references note a much higher + expression pattern in meotheliomas. This may be dependent upon the mix of epithelial and sarcomatous variants.
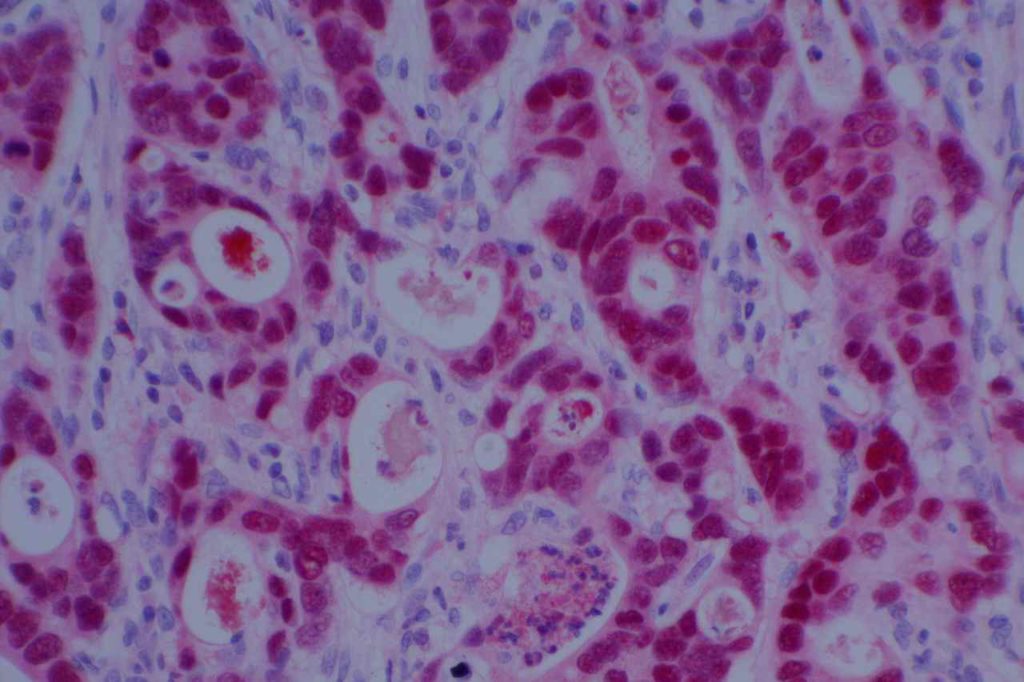
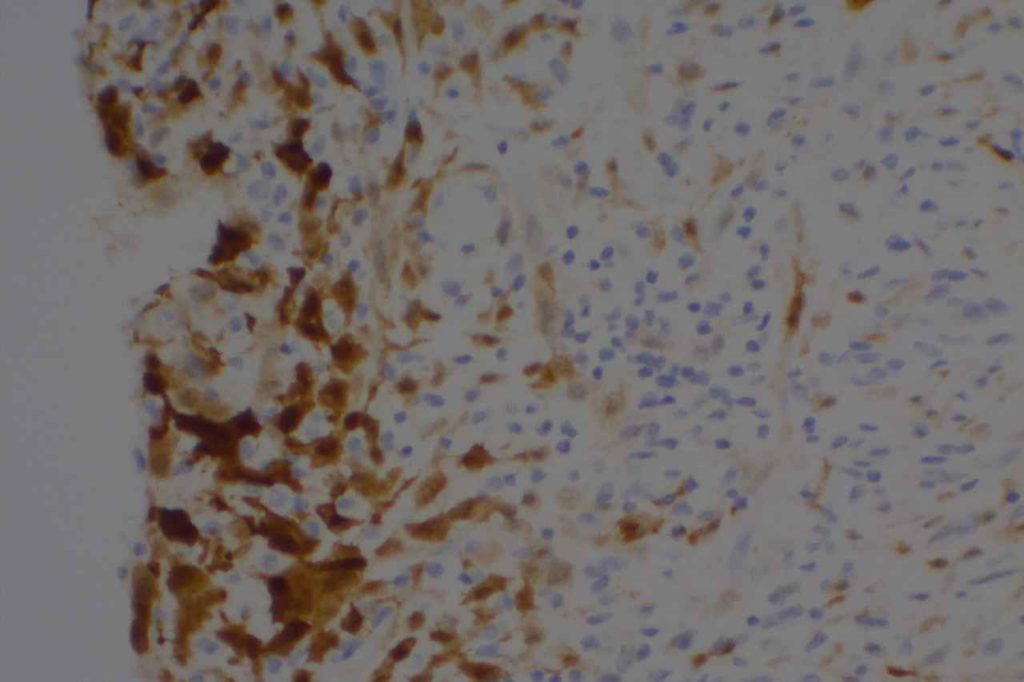
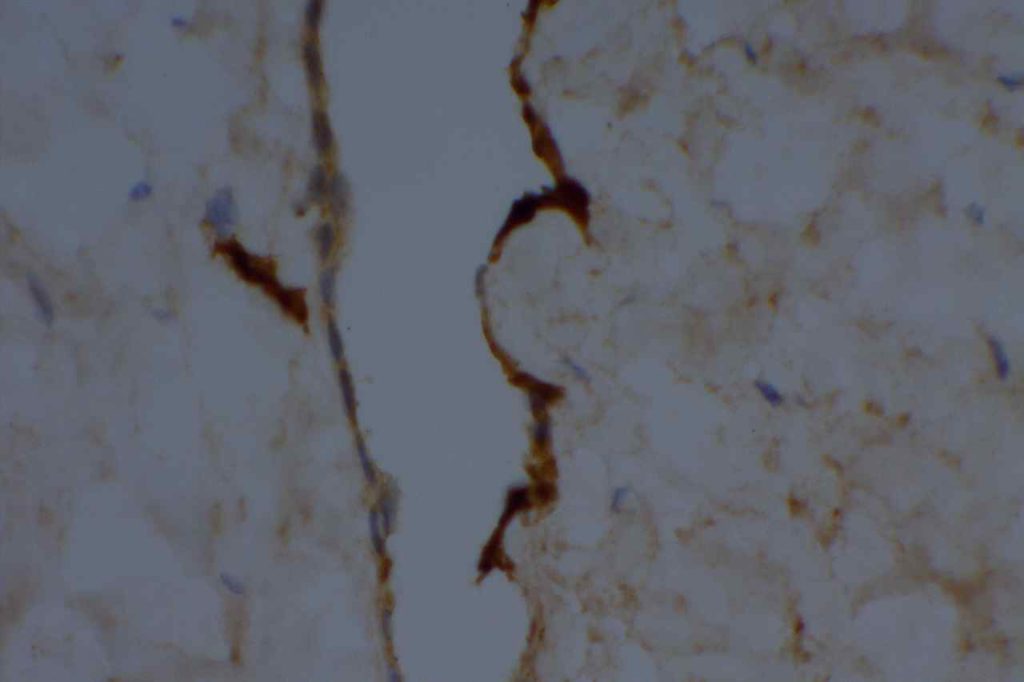
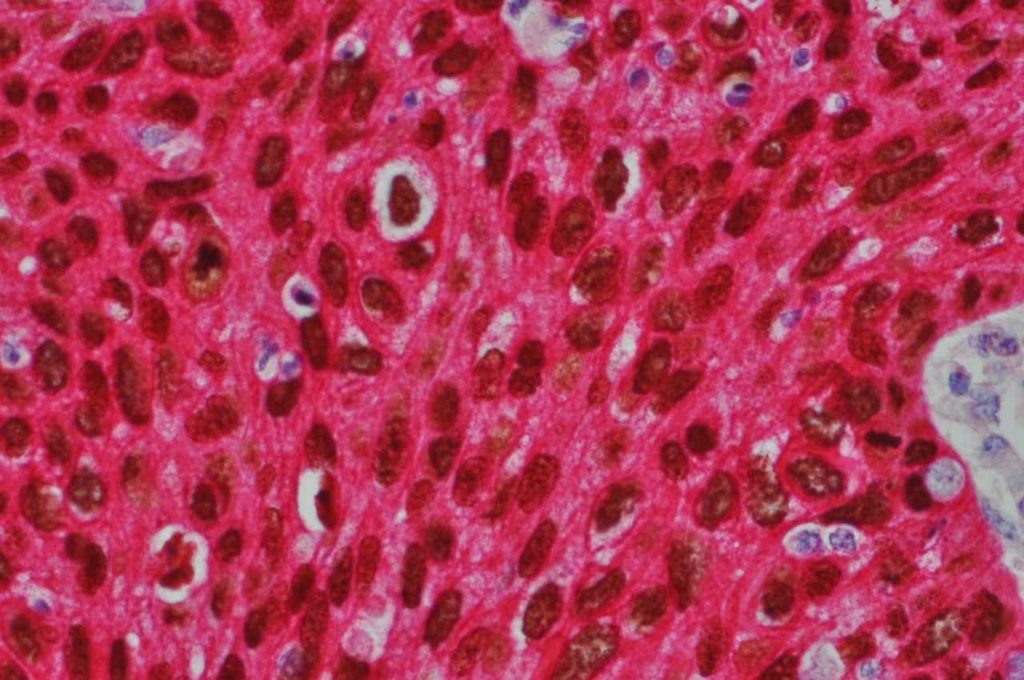
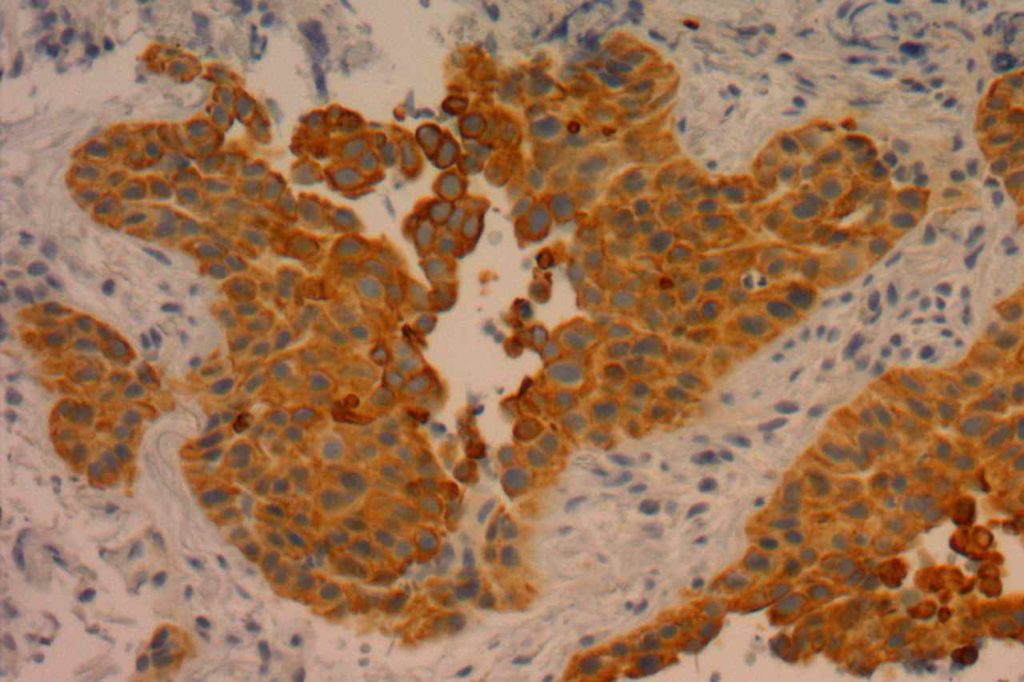
Photomicrographs
Reference
Fichtenbaum EJ, Marsh WL, Zynger DL. CK5, CK5/6, and double-stains CK7/CK5 and p53/CK5 discriminate in situ vs invasive urothelial cancer in the prostate. Am J Clin Pathol. 2012;138: 190–197. doi:10.1309/AJCP5ZC4GQVNWTYR
Bhargava, R., Beriwal, S., Mcmanus, K., & Dabbs, D. J. (2008). CK5 is more sensitive than CK5/6 in identifying the “basal-like” phenotype of breast carcinoma. American Journal of Clinical Pathology, 130(5), 724–730. doi:10.1309/AJCP3KFF1LTYWQIY
Mukhopadhyay, S., & Katzenstein, A.-L. A. (2011). Subclassification of non-small cell lung carcinomas lacking morphologic differentiation on biopsy specimens: Utility of an immunohistochemical panel containing TTF-1, napsin A, p63, and CK5/6. The American Journal of Surgical Pathology, 35(1), 15–25. doi:10.1097/PAS.0b013e3182036d05
Kaufmann, O., Fietze, E., Mengs, J., & Dietel, M. (2001). Value of p63 and cytokeratin 5/6 as immunohistochemical markers for the differential diagnosis of poorly differentiated and undifferentiated carcinomas. American Journal of Clinical Pathology, 116(6), 823–830. doi:10.1309/21TW-2NDG-JRK4-PFJX
Chu, P. G., & Weiss, L. M. (2002). Expression of cytokeratin 5/6 in epithelial neoplasms: an immunohistochemical study of 509 cases. Modern Pathology : an Official Journal of the United States and Canadian Academy of Pathology, Inc, 15(1), 6–10. doi:10.1038/modpathol.3880483
Sutton LM, Han JS, Molberg KH, Sarode VR, Cao D, Rakheja D, et al. Intratumoral expression level of epidermal growth factor receptor and cytokeratin 5/6 is significantly associated with nodal and distant metastases in patients with basal-like triple-negative breast carcinoma. Am J Clin Pathol. 2010;134: 782–787. doi:10.1309/AJCPRMD3ARUO5WPN
Hadi, AIMM Annual Meeting, “The Thirty Most Important Antibodies”, presentation, 2011.
Mod Path 15:6-10, 2002.
Moll R, Divo M, Langbein L. The human keratins: biology and pathology. Histochem Cell Biol. 2008;129: 705–733. doi:10.1007/s00418-008-0435-6