This is considered a provisional entity by the WHO classification in 2008. In many ways this entity is similar clinically to T-LGL leukemia, but there are no rearrangements of immunoglobulin or T-cell receptors since the cells are NK cells.
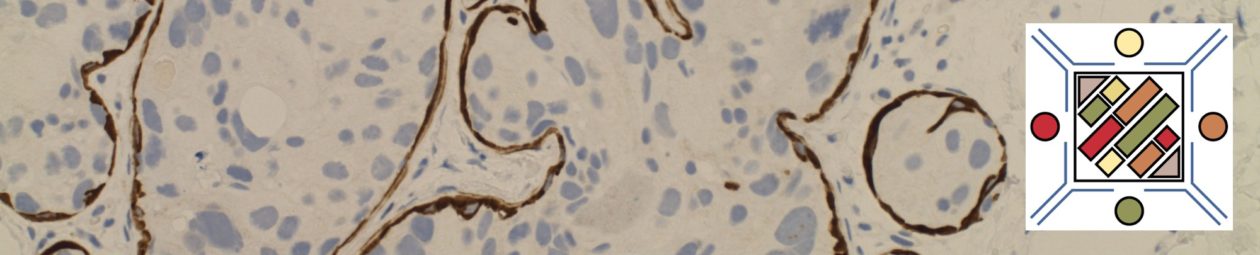
Characteristic Immunophenotypic Profile
|
Marker
|
Comment
|
|
Surface CD3 negative. Cytoplasmic CD3ε is often positive.
|
|
|
Usually weak expression
|
|
|
TIA-1
|
Positive
|
|
Positive
|
|
|
+/- May show diminished of loss of expression.
|
|
|
+/- May show diminished of loss of expression.
|
|
|
CD57
|
+/- May show diminished of loss of expression.
|
|
May show aberrant uniform expression.
|
References
Hematopathology. [edited by] Jaffe, ES. 1st. ed. Elsevier, Inc. © 2011.