Less than 1% of cases of classical Hodgkin lymphoma (CHL) fall into this category. This variant is manifested by numerous Hodgkin’s/ Reed-Sternberg cells without a significant reactive inflammatory infiltrate. These cases can easily be mistaken for other types of malignancy or anapestic large cell lymphoma. Immunophenotyping is critical. EBV infection is present in >90% of cases, And is more common in HIV-positive individuals, older adults, and third world countries. Co-expression of CD30 and PAX-5 is helpful to differentiate from a aplastic large cell lymphoma (ALCL).
Classical Hodgkin Lymphoma – General Information
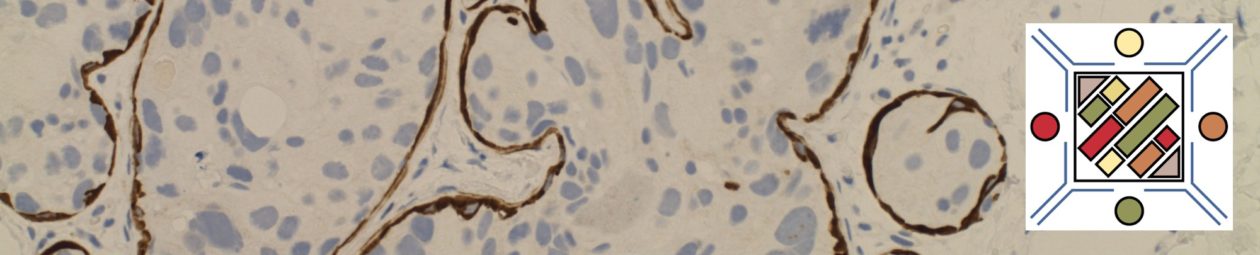
Characteristic Immunohistochemical Features
References
Hematopathology. [edited by] Jaffe, ES. 1st. ed. Elsevier, Inc. © 2011.
Robbins and Cotran Pathologic Basis of Disease. V Kumar, et al. 9th Edition. Elsevier Saunders. 2015.
WHO Classification of Tumors of Haematopoietic and Lymphoid Tissues. SH Swerdlow, et al. International Agency for Research on Cancer. Lyon, 2008.