Myeloid sarcoma is essentially AML occurring outside the bone marrow. It has been referred to by many names including leukemia cutis, granulocytic sarcoma, myeloid sarcoma, and chloroma. Diagnosis may be difficult to make because many of the usual IHC characteristics in the bone marrow are not mirrored when AML presents in the skin or other locations. Additionally, flow cytomtery is often not performed when lesions present in unusual locations (e.g. skin, etc.).
The 2008 WHO Classification lists the following helpful IHC markers from most sensitive to least sensitive: CD68/KP1 > MPO > CD117 > CD99 > CD68/PG-M1 > Lysozyme > CD34 > TdT > CD56 > CD61 > CD30 > CD4.
It is important to remember the individual markers characteristics and that some are less specific than others. It is critical to evaluate the results using a panel of markers combined with the morphology.
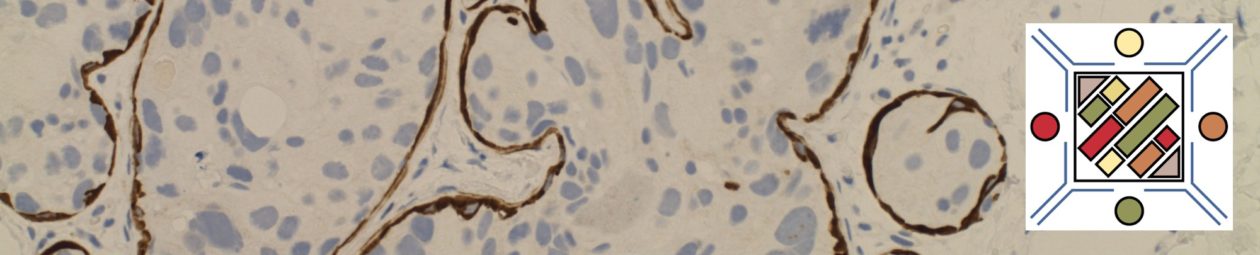
Myeloid Leukemia Cutis
The following is the IHC performance from 33 cases studied at Stanford Medical Center:
|
IHC Marker
|
% Positive
|
|
|
97% (N=33)
|
|
MPO
|
42% (N=33)
|
|
|
94% (N=33)
|
|
CD163
|
25% (N=28)
|
|
|
47% (N=30)
|
|
|
Predominately Negative
|
|
|
Predominately Negative
|
References
Hematopathology. [edited by] Jaffe, ES. 1st. ed. Elsevier, Inc. © 2011.
Cronin DM, et al. Am J Clin Pathol2009, Jul;132(1):101-10.