Key features
- Aggressive course
- High rate of axillary lymph node metastasis (66–100%)
- Morphology– tubulealveolar, morular clusters (spongelike), micropapillary
- Frequent calcifications, including psammoma bodies (42–67%)
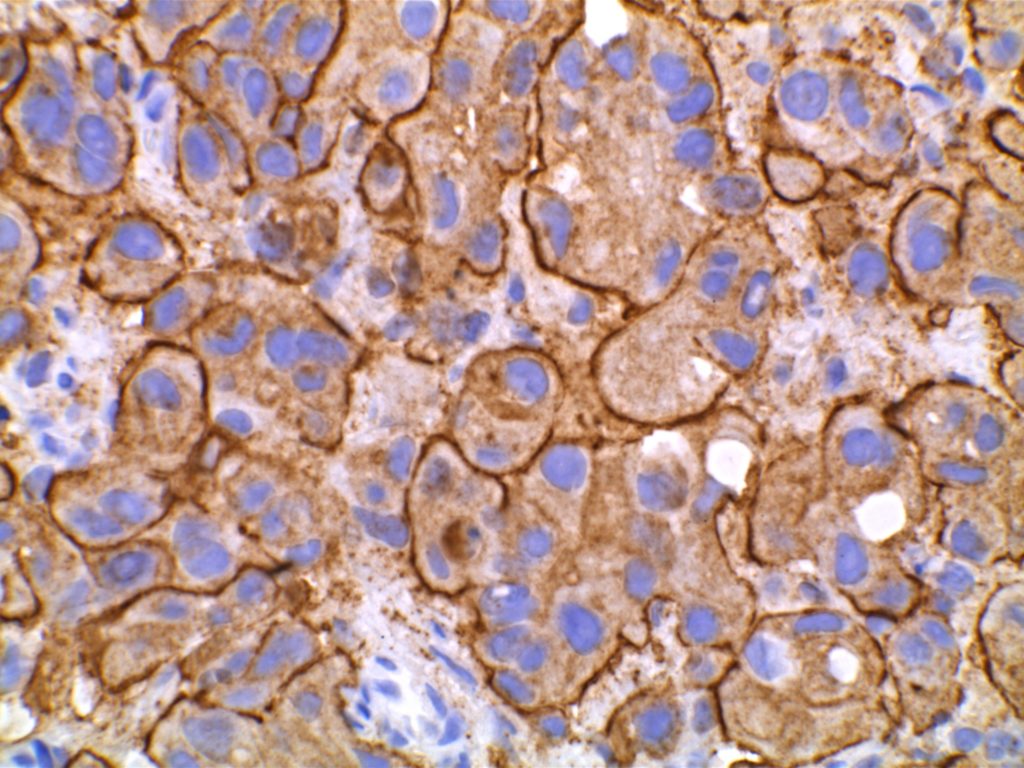
- EMA (epithelial membrane antigen) has reverse membrane staining (outer border of cells)
- Receptor status
Invasive micropapillary carcinoma of the breast is an aggressive variant of ductal carcinoma, and has similar features to micropapillary carcinomas of other sites. Such tumors can either be pure micropapillary carcinomas or only have partial micropapillary differentiation. In either case, both situations are associated with a more aggressive disease course. This tumor is often associated with microcalcifications (including psammomatous calcifications). Pure micropapillary carcinomas account for approximately 2% of breast carcinomas, and breast carcinomas with a component of micropapillary may represent up to 6% of breast carcinoma cases.
Histology
- Anchorage-independent growth
- Cell express E-cadherin and connect to each other, but do not attach to the surrounding stroma
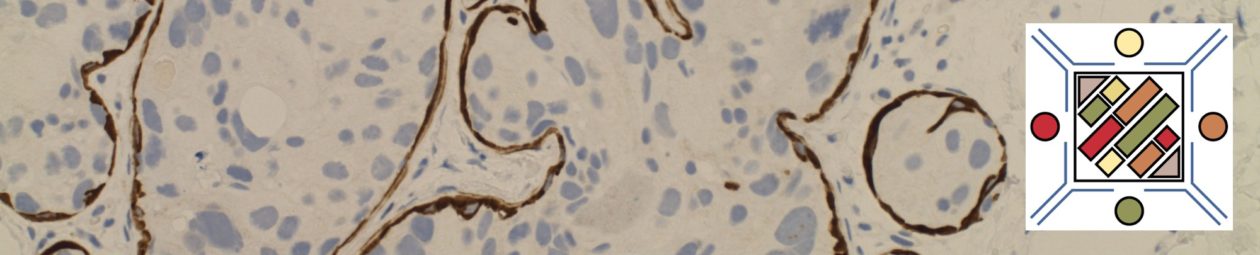
Most cases are mixed with intraductal carcinoma NOS. In the micropapillary areas the morphology is that of micropapillary, tubularalveolar or morular clusters (suspended in clear spaces) having a “spongelike” appearance. The micropapillary clusters lack fibrovascular cores (pseudopapillary). The cytoplasm is granular to dense eosinophilic with intermediate to high grade nuclei. Mitoses are frequent. Particularly characteristic, is the reverse polarity with the apical surface polarized to the outside. This finding is highlighted by EMA (epithelial membrane antigen) showing a reverse membranous staining highlighting the interface with the stroma.
These tumors are associated with a high rate of lymph node metastasis (66–100%). No correlation with the micropapillary component and the frequency of left node metastasis has been identified. These cases appear to have a higher than usual rate of over expression of HER-2/neu.
Photomicrographs


References
Breast Pathology, David Jay Dabbs. 2012, Elsevier Saunders. Pages 559-563.
Kumar, Vinay, Abul K. Abbas, and Jon C. Aster. Robbins and Cotran Pathologic Basis of Disease. Ninth edition. Philadelphia, PA: Elsevier/Saunders, 2015.
Stewart RL, Caron JE, Gulbahce EH, Factor RE, Geiersbach KB, Downs-Kelly E. HER2 immunohistochemical and fluorescence in situ hybridization discordances in invasive breast carcinoma with micropapillary features. Mod Pathol. 2017;30: 1561–1566. doi:10.1038/modpathol.2017.65