Mixed Phenotype Acute Leukemia (MPAL) comprises either blasts with myeloid and lymphoid expression or leukemia with a mixture of myeloblasts and lymphoblasts.
- BIPHENOTYPIC – single population of blasts that express key markers of different lineages (e.g. T-ALL, B-ALL, and/or AML).
- BILINEAL – two cell populations each diagnostic of separate acute leukemia lineages (combined populations ≥20% blasts to met threshold for acute leukemia).
WHO Criteria
- Exclude leukemias with
- t(8;21), t(15;17), inv(16), FGFR mutations/translocations
- Blast phase of CML
- AML with myelodysplastic-related changes (MDS-MRC) , features between MDS-MRC often overlap with MPAL
- Identification of two lineages/mixed phenotype (WHO 2008/2016 Criteria)
WHO Classification
- MPAL with t(9;22)(q34.1;q11.2); BCR-ABL1
- May respond to tyrosine kinase inhibitors (TKIs)
- MPAL with t(v;11q23.3); KMT2A rearranged
- MPAL, B/myeloid, NOS
- Ben conservative when dim (low-level) expression of MPO is the only myeloid feature (not uncommon in cases of B-ALL)
- MPAL, T/myeloid, NOS
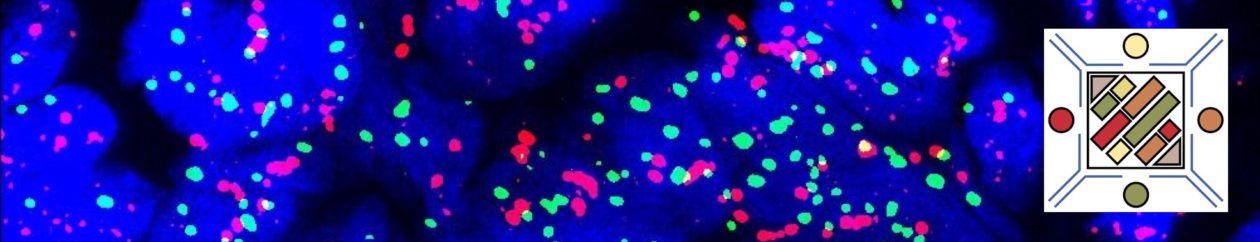
Immunophenotyping for lineage specificity
This is less scientific and more of an expert consensus. Therefore, dependent upon the method of phenotying and consensus method (WHO vs. EGIL), the rate of MPAL varies from ~2% of acute leukemias with the WHO criteria to 3-5% with the EGIL.
WHO 2008/2016 Criteria for Mixed-Phenotype Blasts
- Myeloid
- MPO expression (flow cytometry, immunohistochemistry, or enzyme cytochemistry) – WHO does not define thresholds for positiivity, which can result in variability between laboratories
- Flow cytometry: >10% (some propose 13%) expression compared to isotype control (preferred methodology)
- Enzyme cytochemsitry: >3% staining of blasts
- IHC: No well-defined cutoff (not commonly done – MPO IHC is available)
- (or) monocytic differentiation (≥2 of the following 5)
- NSE cytochemistry
- CD11c, CD14, CD64
- lysozyme
- MPO expression (flow cytometry, immunohistochemistry, or enzyme cytochemistry) – WHO does not define thresholds for positiivity, which can result in variability between laboratories
- T-Lineage
- Strong (equal to or greater than normal lymphocytes) cytoplasmic CD3
- (or) Surface CD3
- B-Lineage
- Strong CD19 plus strong expression of 1 of the following
- CD79a
- Cytoplasmic CD22
- CD10
- (or) Weak CD19 with strong expression in at least 2 of the following
- CD79a
- Cytoplasmic CD22
- CD10
- Strong CD19 plus strong expression of 1 of the following
EGIL Algorithm for Biphenotypic Blasts
General Comments
MPALs have a poorer prognosis compared to other leukemia types, and appear to respond better to ALL-type chemotherapy than AML-type regimens. There may be benefit of allogeneic stem cell transplant in certain circumstances. Some thoughts with regards to why MPAL have a poorer prognosis includes: chemoresistence due to slow replication, phenotype switching of blasts, and high levels of multi drug resistance proteins
References
Charles NJ, Boyer DF. Mixed-Phenotype Acute Leukemia: Diagnostic Criteria and Pitfalls. Arch Pathol Lab Med. 2017;141: 1462–1468. doi:10.5858/arpa.2017-0218-RA
Arber DA, Orazi A, Hasserjian R, Thiele J, Borowitz MJ, Le Beau MM, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127: 2391–2405. doi:10.1182/blood-2016-03-643544
Swerdlow SH, Campo E, Harris, NL, Jaffe ES, Pileri SA, Stein H, Thiele J (Eds): WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues (Revised 4th edition). IARC: Lyon 2017
Bene MC, Castoldi G, Knapp W, et al. Proposals for the immunological classification of acute leukemias: European Group for the Immunological Characterization of Leukemias (EGIL). Leukemia. 1995;9(10):1783–1786.