Nodular Lymphocyte Predominate Hodgkin Lymphoma (NLPHL) epresents approximately 5-10% of Hodgkin lymphoma cases (predominately male, 30-50 y/o) and has slightly different appearing neoplastic cells (popcorn cells – folded/multilobuated usually with multiple nucleoli). The cellular background is typically composed of small lymphocytes and histiocytes. Some plasma cells may be present at the peripheral of the nodule. Neutrophils and eosinophils are not typically present. The immunophenotype of lymphocyte predominate (LP) cells in NLPHL is different from classical Hodgkin lymphoma. The LP cells express CD20 and BCL 6, but are typically negative for CD30 and CD15. Dim expression of CD30 can be seen.
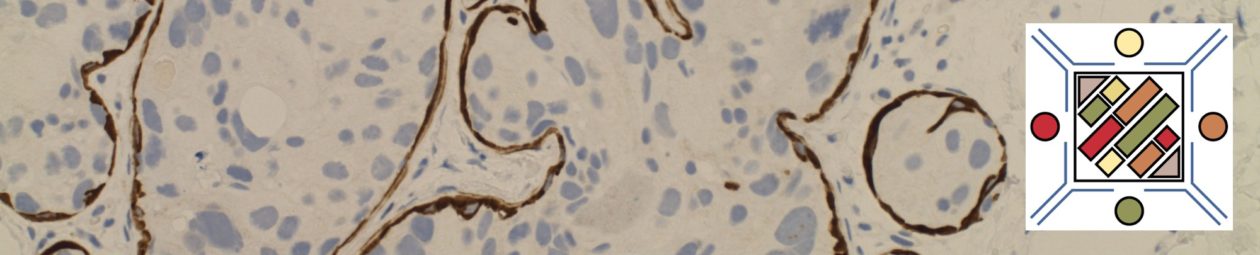
A critically important aspect of this diagnosis is identification of nodularity. There is significant morphologic and molecular overlap between NLPHL and T-cell/histiocyte-rich large B-cell lymphoma. Both of these entities share a common immunophenotype and neoplastic cell morphology, but the latter is a diffuse process were as NLPHL shows at least partial modularity. This differentiation may not be possible on a small biopsy sample. CD21 (follicular dendritic cell marker) may be helpful to demonstrate expansion of germinal center areas, which is the location of the neoplastic cell in NLPHL.
EBV infection is NOT characteristic of this Hodgkin lymphoma subtype. Not infrequently lymph nodes will also have evidence of progressive transformation of germinal centers (PTGC) adjacent to NLPHL. It is not clear if this is a pre-malignant condition, although most cases of PTGC do not develop into Hodgkin lymphoma.
Clinically, it is important to differentiate classical Hodgkin lymphoma and NLPHL due to treatment regimen differences. These lymphomas while both sharing relatively good prognosis, should be thought of as completely different entities. Interestingly, in some countries localized stage I NLPHL is treated by local excision without further therapy unless there is a recurrence.
Morphologic Patterns
- PATTERN A – “Classical” B-Cell rich, Nodular
- PATTERN B – Serpiginous/Interconnected
- PATTERN C – Prominent Extra-Nodular L&H Cells
- PATTERN D – T-Cell Rich, Nodular
- PATTERN E – Diffuse (TCRBCL or DLBCL-Like)
- PATTERN F – Diffuse moth-eaten, B-Cell Rich
Immuonphenotype
|
Negative in the lymphoma cells, but will often show ringing by CD3+ T-cells.
|
|
|
Positive in the lymphoma cells (strong membrane staining), and also stains many of the cells in the nodular region that contain the lymphoma cells.
|
|
|
Positive in the lymphoma cells.
|
|
|
Positive in the lymphoma cells.
|
|
|
Positive in the lymphoma cells. This is in contrast to classical Hodgkin lymphoma, which is negative for CD45.
|
|
|
Positive in >50%; Membranous and Golgi region dot-like positivity.
|
|
|
OCT-2
|
Co-expressed in NLPHL; in contrast to CHL.
|
|
Negative in the lymphoma cells.
|
|
|
Negative in the lymphoma cells (rarely can have weak expression). Adjacent benign immunoblasts will express CD30. Be careful to clarify which cells are positive.
|
|
|
Very helpful in demonstrating the follicular dendritic meshwork, in which the lymphoma cells are embedded.
|
|
|
CD57
|
May label CD3+ T-cells in the nodular areas and ringing the lymphoma cells.
|
NLPHL vs. T-Cell/Histocyte-Rich Large B-Cell Lymphoma (THRLBCL)
- NLPHL arises in a follicular dendritic meshwork (CD21+)
- NLPHL has a background of small B-lymphocytes and CD4+/CD57+ T-cells
- THRLBCL typically has a background of CD8+/TIA-1 positive cells and absence of small B-lymphoctyes
- NLPHL rarely has bone marrow involvement, and THRLBCL often presents with advanced disease
- There is an overlap between NLPHL and THRLBCL that cannot be definitely excluded (further supported by similar gene expression profiling studies).
- The identification of lymphocyte predominant (LP) cells with B-cells in a follicle structure (i.e. CD21 dendritic meshwork) is adequate to exclude the diagnosis of THRLBCL.
References
Smith LB. Nodular lymphocyte predominant Hodgkin lymphoma: diagnostic pearls and pitfalls. Arch Pathol Lab Med. 2010;134: 1434–1439.
Zhao FX. Nodular lymphocyte-predominant hodgkin lymphoma or T-cell/histiocyte rich large B-cell lymphoma: the problem in “grey zone” lymphomas. Int J Clin Exp Pathol. 2008;1: 300–305.
Rets AV, Gottesman SRS. Nodular Lymphocyte Predominant Hodgkin Lymphoma versus T-Cell/Histiocyte-Rich Large B-Cell Lymphoma: A Diagnostic Challenge. Case Rep Pathol. 2014;2014: 956217–5. doi:10.1155/2014/956217
Hematopathology. [edited by] Jaffe, ES. 1st. ed. Elsevier, Inc. © 2011.
Robbins and Cotran Pathologic Basis of Disease. V Kumar, et al. 9th Edition. Elsevier Saunders. 2015.
Swerdlow SH, Campo E, Harris, NL, Jaffe ES, Pileri SA, Stein H, Thiele J (Eds); WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues (Revised 4th edition). IARC: Lyon 2017