2016 WHO Classification
- Solitary Plasmacytoma of Bone
- Extra-osseous Plasmacytoma
Solitary Plasmacytoma of Bone
- Modest elevations of M protein in serum or urine in a subset of patients (24-72%).
- Localized collection of monoclonal plasma cells (plasmacytoma), without evidence of systemic disease.
- Normal random bone marrow biopsy without clonal plasma cells.
- Normal skeletal survey and MRI or CT
- Abence of end organ damage (defines multiple myeloma)
- Osseous plasmacytomas have a very high risk of progressing to multiple myeloma (though this can take up to 20 years or longer).
- Up to 2/3rds will progress
- 10% will progress within 3 years
Solitary Plasmacytoma with minimal bone marrow involvement – is defined by <10% clonal plasma cells in a random bone marrow biopsy. Approximately 60% of these patients will progress to plasma cell myeloma in 3 years.
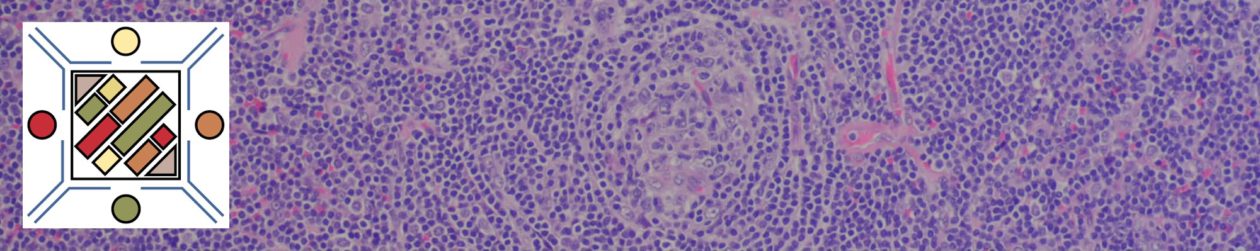
Extra-osseous Plasmacytoma
- Modest elevations of M protein in serum or urine (often IgA) in a subset of patients (20%).
- Localized collection of monoclonal plasma cells (plasmacytoma), without evidence of systemic disease.
- Normal random bone marrow biopsy without clonal plasma cells.
- Normal skeletal survey and MRI or CT
- Absence of end organ damage (defines multiple myeloma)
- Non-osseous plasmacytomas have a very low risk of progressing to multiple myeloma (~15%) and are often cured by local excision or radiation (~25% regional recurrence rate).
- May be challenging to differentiate from a lymphoma with prominent plasmacytic differentiation
- Atypical/blastic appearance would favor a multiple myeloma or plasmablastic lymphoma.
- Evidence of a monoclonal lymphoid population (flow cytometry) would support a lymphoma with plasmacytic differentiation.
- Sometimes it is not possible to definitively differentiate between a plasmacytoma and lymphoma with plasmacytic differentiation.
- Immunophenotype
- Cyclin D1 – Negative
- CD56 – ~1/3rd may have weak expression (multiple myeloma – 71%+)
- CD45 – 91% positive (multiple myeloma – 41%+)
- CD19 – 95% positive (multiple myeloma – 10%+)
References
Robbins and Cotran Pathologic Basis of Disease. V Kumar, et al. 9th Edition. Elsevier Saunders. 2015. pp. 599-601.
WHO Classification of Tumors of Haematopoietic and Lymphoid Tissues. SH Swerdlow, et al. International Agency for Research on Cancer. Lyon, 2008. pp. 200-213
Swerdlow SH, Campo E, Pileri SA, Harris NL, Stein H, Siebert R, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127: 2375–2390. doi:10.1182/blood-2016-01-643569