Major Criteria
- Presence of JAK2, CALR, or MPL mutation, (or) presence of other clonal marker (or) absence of reactive fibrosis
- Does not meet WHO criteria for another myeloid/myeloproliferative neoplasm
- Presence of an atypical megakaryocytic proliferation and grade 2-3 fibrosis (MF2-3)
Minor Criteria
Presence of at least one of the following on two consecutive studies:
- Leukoerythroblastosis
- Splenomegaly (palpable)
- Leukocytosis (>11,000/μL)
- Anemia (not caused by another condition)
- Elevated LDH
Diagnosis of PMF requires meeting all three major criteria and at least one minor criteria.
Pre-fibrotic Myelofibrosis (pre-PMF)
- Same criteria as PMF, except fibrosis is MF1 or less, and leukoerythroblastosis is not included in the minor criteria
- In contrast the ET, pre-PMF is hypercellular for age with an increased granulocytic component (erythroid component is often decreased).
Frequency of Molecular Abnormalities
- JAK2 – 57-58% (V617F mutations)
- CALR – 15-25%
- MPL – 8-9%
Overall, approximately 80-91% of cases of PMF have either a JAK2, CALR, or MPL mutation.
Myelofibrosis Grading
|
Grade
|
Comment
|
|
Scattered linear fibers without intersections. Normal bone marrow.
|
|
|
MF1
|
Loose network of reticulin fibers with intersections (particularly perivascular)
|
|
Diffuse increase of reticulin fibers with increased density and numerous intersections. Focal bundles of thick fibers.
|
|
|
Diffuse increase of reticulin fibers with increased density and numerous intersections. Increased thick bundles of fibers consistent with collagen fibrosis. Osteosclerosis usually present.
|
In cases of MF2 or MF3, it is recommended to perform trichrome stain to evaluate for collagen fibrosis.
MF – Accelerated phase = 10-19% blasts in the peripheral blood and/or the bone marrow.
MF – Acute Transformation = ≥20% blasts in the blood or bone marrow.
Treatment – JAK 1/2 inhibitor ruxolitinib/Jakafi®
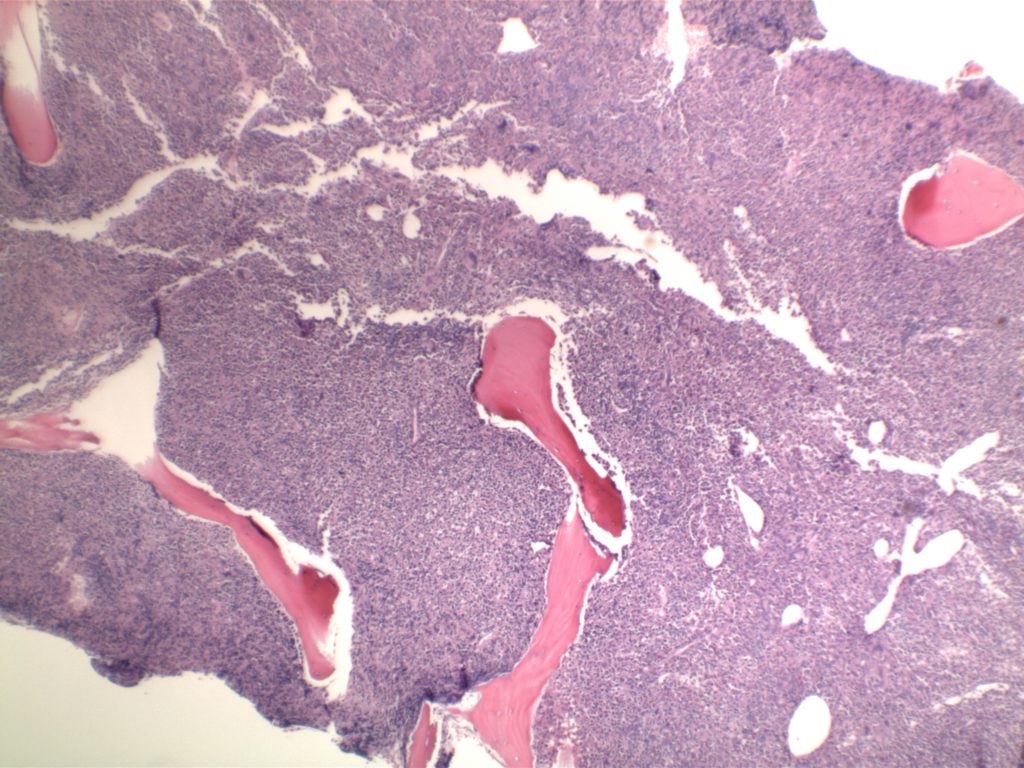
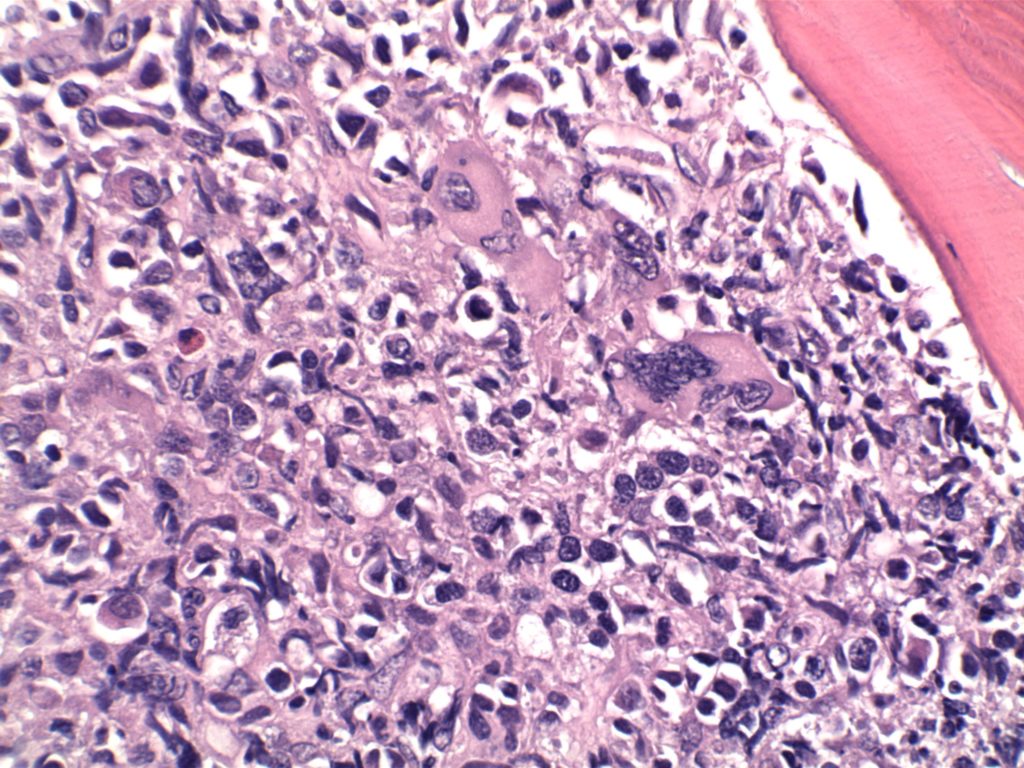
Photomicrographs
Immunohistochemistry
The use of immunohistochemistry (IHC) in many of the myeloproliferative neoplasms is limited. Identifying an increased blast population is one of the most useful, and may indicate a more aggressive course or transformation to acute leukemia. Helpful IHC markers may include:
|
Stain
|
Comment
|
|
CD34 marks immature cells including myeloblasts. In the setting of AML, it is ~70% sensitive. A subset of lymphoblasts may express CD34.
|
|
|
CD117 is a specific myeloid marker, and marks a subset of myeloblasts. The expression is dim, and one often must look at 20-40X to clearly see expression. Mast cells (fried egg looking cell) will have very strong expression.
|
|
|
CD71 marks nucleated erythroid cells. This may be helpful in quantitating and differentiating erythroid cells from myeloid cells. This marker may be set-up as a double stain with CD34.
|
|
|
In the setting of hematopoietic cells, E-Cadherin marks immature erythroid cells. Like CD71, E-Cadherin may be useful to differentiate immature erythroid cells from immature myeloid cells.
|
|
|
TdT is a sensitive lymphoblast (~95%) marker. It is not entirely specific for lymphoblasts, but other markers can help clarify diagnostic difficulties (B and T-cell markers).
|
References
Swerdlow SH, Campo E, Harris, NL, Jaffe ES, Pileri SA, Stein H, Thiele J (Eds): WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues (Revised 4th edition). IARC: Lyon 2017
Arber DA, Orazi A, Hasserjian R, Thiele J, Borowitz MJ, Le Beau MM, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127: 2391–2405. doi:10.1182/blood-2016-03-643544
Kim SY, Im K, Park SN, Kwon J, Kim J-A, Lee DS. CALR, JAK2, and MPL mutation profiles in patients with four different subtypes of myeloproliferative neoplasms: primary myelofibrosis, essential thrombocythemia, polycythemia vera, and myeloproliferative neoplasm, unclassifiable. Am J Clin Pathol. 2015;143: 635–644. doi:10.1309/AJCPUAAC16LIWZMM
Tefferi A, Lasho TL, Finke CM, Knudson RA, Ketterling R, Hanson CH, et al. CALR vs JAK2 vs MPL-mutated or triple-negative myelofibrosis: clinical, cytogenetic and molecular comparisons. Leukemia. 2014;28: 1472–1477. doi:10.1038/leu.2014.3
Hematopathology. [edited by] Jaffe, ES. 1st. ed. Elsevier, Inc. © 2011.